Incidence and risk for Cement Implantation Syndrome after hemiarthroplasty
Abstract
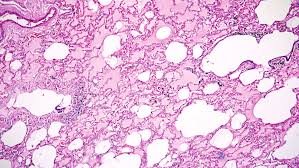
Background: Bone Cement Implantation Syndrome (BCIS) is a highly under-reported rare fatal complication of cementation, characterized by hypoxia, hypotension, cardiac arrhythmias, and cardiac arrest. With aim to alert surgeons about rare, but serious harm due to BCIS and its risk, clinical features, preventive measures and management, we evaluated the incidence and risk factor associated for BCIS in cemented hemiarthroplasty for fractures around hip.
Material & methods: All patients of fracture neck of femur or intertrochanteric, operated with cemented hemiarthroplasty, who sustained BCIS during or within 24 hrs of the cementation were included in the study. The BCIS was diagnosed, when the patient had hypoxia (SpO2 <94%) or fall in systolic blood pressure > 20mm. these patients were evaluated for presence of risk factors like age, sex, osteoporosis, use of diuretics, poor preexisting physical reserve, pre-operative cardiopulmonary function etc.
Results: In 430 patients of cemented hemiarthroplasty done of fractures around hip, 13 sustained BCIS. The mean age in these patients was 84.3 years. Severity was grade 1 in 7 patients, grade 2 in 4 patients and grade 3 in 2 patients. All the patients of the grade 1 and grade 2 were revived successfully, whereas none of the patients of the grade 3, could be revived. Age and poor cardiac reserves were most commonly associated with BCIS.
Conclusion: BCIS is a rare, preventable, fatal complication of cementation which can diagnosed early by constant monitoring. Management is supportive and preventive is best way by surgical modification with modern cementing techniques, especially in high risk patients.
Downloads
References
2. Donaldson AJ, Thomson HE, Harper NJ, Kenny NW. Bone cement implantation syndrome. Br J Anaesth. 2009;102(1):12-22.
3. Parvizi J, Holliday AD, Ereth MH, et al. Sudden death during primary hip arthroplasty. Clin Orthop Relat Res 1999 Dec;(369):39-48.
4. Orsini EC, Richards RR, Mullen JM. Fatal fat embolism during cemented total knee arthroplasty: a case report. Can J Surg 1986; 29: 385–6.
5. Chen HL, Wong CS, Ho ST, Chang FL, Hsu CH, Wu CT. A lethal pulmonary embolism during percutaneous vertebroplasty. Anesth Analg 2002; 95: 1060–2
6. Jain S, Solanki M, Pal R, Rohra S. Bone cement implanation syndrome during cemented hemiarthroplasty and review of literature. J Orthop Edu. 2016;2;2;69-73.
7. Govil P, Kakar PN, Arora D, Das S, Gupta N, Govil D, Gupta S, Malohtra A, Bone Cement Implantation Syndrome: A Report of Four Cases. Ind J of Anaesth.
2009;53(2):214-218.
8. Patterson B, Healey J, Cornell C, Sharrock N. Cardiac arrest during hip arthroplasty with a cemented long-stem component. A report of seven cases. J Bone Joint Surg 1991; 73: 271–7.
9. Orsini EC, Byrick RJ, Mullen JB, Kay JC, Waddell JP. Cardiopulmonary function and pulmonary microemboli during arthroplasty using cemented or non-cemented components. The role of intramedullary pressure. J Bone Joint Surg. 1987;69:822-832.
10. Tryba M, Linde I, Voshage G, Zenz M. Histamine release and cardiovascular reactions to implantation of bone cement during total hip replacement. Anaesthetist 1991;40:25–3.
11. Motobe T, Hashiguchi T, Uchimura T, et al. Endogenous cannabinoids are candidates for lipid mediators of bone cement implantation syndrome. Shock 2004;21:8–12.
12. Lewis RN. Some studies of the complement system during total hip replacement using bone cement under general anaesthesia. Eur J Anaesth 1997;14:35–9.
13. Modig J, Busch C, Waernbaum G. Effects of graded infusion of monomethylmethacrylate on coagulation, blood lipids, respiration and circulation. Clin Orthop Relat Res 1975; 113: 187–95
14. Hayakawa M, Fujioka Y, Morimoto Y, Okamura A, Kemmotsu O. Pathological evaluation of venous emboli during total hip arthroplasty. Anaesthesia 2001; 56: 571–5.
15. Griffiths R, Parker M. Bone cement implantation syndrome and proximal femoral fracture. Br J Anaesth 2015; 114; 6-7.
16. Hayakawa M, Fujioka Y, Morimoto Y, Okamura A, Kemmotsu O. Pathological evaluation of venous emboli during total hip arthroplasty. Anaesthesia 2001; 56: 571–5.
17. Ereth MH, Weber JG, Abel MD, et al. Cemented versus noncemented total hip arthroplasty-embolism, haemodynamics and intrapulmonary shunting. Mayo Clinic Proc 1992; 67: 1066–74.
18. Lafont ND, Kostucki WM, Marchand PH, Michaux MN, Boogaerts JG. Embolism detected by transoesophageal echocardiography during hip arthroplasty. Can J Anaesth 1994; 41: 850–3.
19. Byrick RJ. Cement implantation syndrome: a time limited embolic phenomenon. Can J Anaesth.1997;44:107–11.
20. National Patient Safety Agency. Mitigating surgical risk in patients undergoing hip arthroplasty for fractures of the proximal femur, 2009. http://www.nrls.npsa.nhs.uk/alerts/?entryid45=59867
The entire contents of the Orthopaedic Journal of Madhya Pradesh Chapter are protected under Indian and International copyrights. Orthopaedic Journal of Madhya Pradesh Chapter allow authors to retain the copyrights of their papers without restrictions, Authors grant the publisher the right of exclusive publication. The Journal then grants to all users a free, irrevocable, worldwide, perpetual right of access to, and a license to copy, use, distribute, perform and display the work publicly and to make and distribute derivative works in any digital medium for any reasonable non-commercial purpose, subject to proper attribution of authorship. The journal also grants the right to make numbers of printed copies for their personal non-commercial use under Creative Commons Attribution-Non-commercial share alike 4.0 International Public License.
 OAI - Open Archives Initiative
OAI - Open Archives Initiative












