A Prospective Analysis of Functional Outcome of Surgical Stabilization of Distal End Radius fractures with Plate Osteosynthesis
Abstract
Introduction: Distal radius fractures (DRF) are the most common fractures of the upper extremities and due to population explosion, with an ageing society & enormous increase of high-speed motor vehicle accidents, the number of distal radial fractures can be expected to increase in the coming decades. Plate osteosynthesis has become the standard treatment for comminuted intra articular DRF. Main aim of this study was to analyse the functional outcome in patients stabilized by plate osteosynthesis with minimum follow up of 6 months.
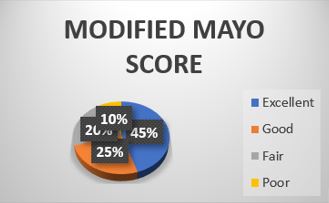
Material and Methods: A prospective study was done on 46 patients with distal radius fractures who were operated with plate osteosynthesis, type of plate was decided as per fracture pattern and followed up at 1, 3, and 6 months and outcomes measured using Modified Mayo score, Grip strength tested by Dynamometer.
Observations: Volar plating was done in 34 patients; dual plating was done in 4 patients dorsal column plating was done in 8 patients. Average time of radiological union of fracture was 10 weeks, average time of clinical union of fractures was 8 weeks, average time to return to normal activity was 3 weeks, average time to return to professional activity was 4 weeks.
Results: According to Modified MAYO score 18 patients had excellent results, 10 had good results, 8 had fair and 4 had poor results. Grip strength was >80% compared to normal side in 29 patients, >60% in 8 patients and, <60% compared to normal side in 3 patients measured with a Dynamometer at 6 months.
Conclusion: Fractures of distal end radius managed with plate osteosynthesis is a good treatment modality with excellent results provided the surgeon has a sound knowledge of literature and a good surgical hand.
Downloads
References
MacIntyre NJ, Dewan N (2016) Epidemiology of distal radius fractures and factors predicting risk and prognosis. J Hand Ther 29:136–145.
Figl M, Weninger P, Liska M et al (2009) Volar fixed-angle plate osteosynthesis of unstable distal radius fractures: 12 months results. Arch Orthop Trauma Surg 129:661–669.
Figl M, Weninger P, Jurkowitsch J et al (2010) Unstable distal radius fractures in the elderly patient-volar fixed-angle plate osteosynthesis prevents secondary loss of reduction. J Trauma Inj Infect Crit Care 68:992–998.
Gologan RE, Koeck M, Suda AJ, Obertacke U (2019) %3e 10-year outcome of dislocated radial fractures with concomitant intracarpal lesions as proven by MRI and CT. Arch Orthop Trauma Surg 139:877–881.
Esenwein P, Sonderegger J, Gruenert J et al (2013) Complications following palmar plate fixation of distal radius fractures: a review of 665 cases. Arch Orthop Trauma Surg 133:1155–1162.
Le ZS, Kan SL, Su LX, Wang B (2015) Meta-analysis for dorsally displaced distal radius fracture fixation: volar locking plate versus percutaneous Kirschner wires. J Orthop Surg Res.
Quadlbauer S, Pezzei C, Jurkowitsch J et al (2018) Early complications and radiological outcome after distal radius fractures stabilized by volar angular stable locking plate. Arch Orthop Trauma Surg 138:1773–1782.
Quadlbauer S, Pezzei C, Jurkowitsch J et al (2016) Early rehabilitation of distal radius fractures stabilized by volar locking plate: a prospective randomized pilot study. J Wrist Surg 06:102–112.
Lozano-Calderón SA, Souer S, Mudgal C et al (2008) Wrist mobilization following volar plate fxation of fractures of the distal part of the radius. J Bone Jt Surg Ser A 90:1297–1304.
Osada D, Kamei S, Masuzaki K et al (2008) Prospective study of distal radius fractures treated with a volar locking plate system. J Hand Surg Am 33:691–700.
Lameijer CM, ten Duis HJ, van Dusseldorp I et al (2017) Prevalence of posttraumatic arthritis and the association with outcome measures following distal radius fractures in non-osteoporotic patients: a systematic review. Arch Orthop Trauma Surg 137:1499–1513.
Arora R, Lutz M, Deml C et al (2011) A Prospective randomized trial comparing nonoperative treatment with volar locking plate fxation for displaced and unstable distal radial fractures in patients sixty-fve years of age and older. J Bone Jt Surg Am 93:2146–2153.
Arora R, Lutz M, Hennerbichler A et al (2007) Complications following internal fxation of unstable distal radius fracture witha palmar locking-plate. J Orthop Trauma 21:316–322.
Haug LCP, Deml C, Blauth M, Arora R (2011) Dorsal screw penetration following implant removal after volar locked plating of distal radius fracture. Arch Orthop Trauma Surg 131:1279–1282.
Erhart S, Toth S, Kaiser P et al (2018) Comparison of volarly and dorsally displaced distal radius fracture treated by volar locking plate fixation. Arch Orthop Trauma Surg 138:879–885.
Veldman PH, Reynen HM, Arntz IE, Goris RJ (1993) Signs and symptoms of refex sympathetic dystrophy: prospective study of 829 patients. Lancet (London, England) 342:1012–1016.
Crijns TJ, van der Gronde BATD, Ring D, Leung N (2018) Complex regional pain syndrome after distal radius fracture is uncommon and is often associated with fibromyalgia. Clin Orthop Relat Res 476:744–750.
Ng CY, McQueen MM (2011) What are the radiological predictors of functional outcome following fractures of the distal radius? J Bone Joint Surg Br 93(B):145–150.
Schmitt R, Pommersberger K (2014) Karpale Funktion und Morphometerie. In: Schmitt R, Lanz U (eds) Bildgebende Diagnostik der Hand, 3rd edn. Thieme, Germany, pp 184–197.
Soong M, Earp BE, Bishop G et al (2011) Volar locking plate implant prominence and flexor tendon rupture. J Bone Jt Surg Ser A 93:328–335.
Schlickum L, Quadlbauer S, Pezzei C et al (2018) Three-dimensional kinematics of the fexor pollicis longus tendon in relation to the position of the FPL plate and distal radius width. Arch Orthop Trauma Surg.
Pillukat T, Fuhrmann R, Windolf J, van Schoonhoven J (2016) Die palmare winkelstabile Plattenosteosynthese bei Extensions frakturen des distalen Radius. Oper Orthop Traumatol 28:47–64.
Zhang B, Chang H, Yu K et al (2017) Intramedullary nail versus volar locking plate fxation for the treatment of extra-articular or simple intra-articular distal radius fractures: systematic review and meta-analysis. Int Orthop 41:2161–2169.
Quadlbauer S, Pezzei C, Jurkowitsch J et al (2020) Rehabilitation after distal radius fractures - is there a need for immobilization and physiotherapy Arch Orthop Trauma Surg.
Alter TH, Sandrowski K, Gallant G et al (2019) Complications of volar plating of distal radius fractures: a systematic review. J Wrist Surg 08:255–262.
Orbay JL, Fernandez DL (2002) Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg Am 27:205–215.
Orbay JL, Fernandez DL (2004) Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg Am 29:96–102.
Soong M, Van Leerdam R, Guitton TG et al (2011) Fracture of the distal radius: risk factors for complications after locked volar plate fixation. J Hand Surg Am 36:3–9.
Quadlbauer S, Leixnering M, Rosenauer R et al (2020) Palmar radioscapholunate arthrodesis with distal scaphoidectomy. Oper Orthop Traumatol.
Roh YH, Lee BK, Noh JH et al (2014) Factors associated with complex regional pain syndrome type I in patients with surgically treated distal radius fracture. Arch Orthop Trauma Surg 134:1775–1781.
Üçeyler N, Eberle T, Rolke R et al (2007) Differential expression patterns of cytokines in complex regional pain syndrome. Pain 132:195–205.
Tanl ECT, Janssenl AJM, Roestenbergl P et al (2011) Mitochondrial dysfunction in muscle tissue of complex regional pain syndrome type I patients. Eur J Pain 15:708–715.
The entire contents of the Orthopaedic Journal of Madhya Pradesh Chapter are protected under Indian and International copyrights. Orthopaedic Journal of Madhya Pradesh Chapter allow authors to retain the copyrights of their papers without restrictions, Authors grant the publisher the right of exclusive publication. The Journal then grants to all users a free, irrevocable, worldwide, perpetual right of access to, and a license to copy, use, distribute, perform and display the work publicly and to make and distribute derivative works in any digital medium for any reasonable non-commercial purpose, subject to proper attribution of authorship. The journal also grants the right to make numbers of printed copies for their personal non-commercial use under Creative Commons Attribution-Non-commercial share alike 4.0 International Public License.
 OAI - Open Archives Initiative
OAI - Open Archives Initiative












