Is It Worthy To Replace Hip Than To Go For Intramedullary Osteosynthesis In Unstable Intertrochantric Fractures In Elderly- A Prospective Comparative Study
Sabir A1, Mohan R2, Faizan M3*, Jilani L4, Ahmed S5, Shaan Z6
1 AB Sabir, Department of Orthopaedics Surgery, Jawahar Lal Nehru Medical College Aligarh Muslim University, Aligarh, Uttar Pradesh, India.
2 R Mohan, Department of Orthopaedics Surgery, Jawahar Lal Nehru Medical College Aligarh Muslim University, Aligarh, Uttar Pradesh, India.
3* Mohd Faizan, Assistant Professor, Department of Orthopaedics Surgery, Jawahar Lal Nehru Medical College Aligarh Muslim University, Aligarh, Uttar Pradesh, India.
4 LZ Jilani, Department of Orthopaedics Surgery, Jawahar Lal Nehru Medical College Aligarh Muslim University, Aligarh, Uttar Pradesh, India.
5 S Ahmed, Department of Orthopaedics Surgery, Jawahar Lal Nehru Medical College Aligarh Muslim University, Aligarh, Uttar Pradesh, India.
6 ZH Shaan, Department of Orthopaedics Surgery, Jawahar Lal Nehru Medical College Aligarh Muslim University, Aligarh, Uttar Pradesh, India.
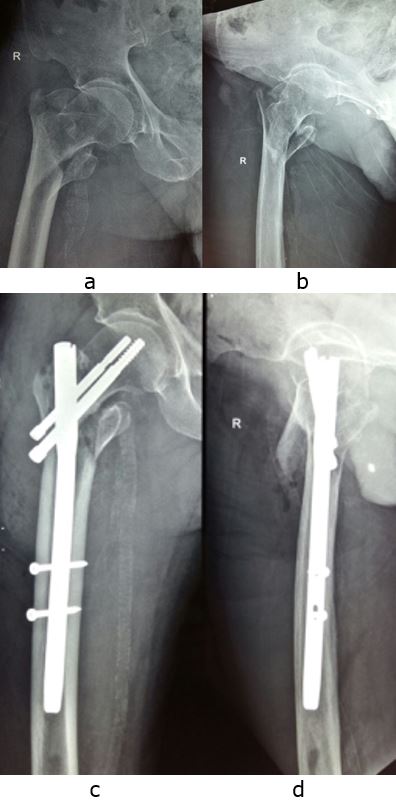
Background: Internal fixation for the management of unstable intertrochantric femoral fractures in elderly is difficult and less successful due to communition and poor bone stock. Arthroplasty for unstable intertrochantric fracture in elderly has produced promising results as per literature. So, we conducted this study to compare the results of intramedullary devices with cemented bipolar hemiarthroplasty in unstable osteoporotic intertrochanteric fractures in elderly patients.
Material and methods: 51 patients, 65 years or older with unstable osteoporotic intertrochanteric femoral fractures were treated with internal fixation or hemiarthroplasty. Intraoperative parameters and functional outcome as per Harris Hip Score were compared.
Results: Average age of patients for intramedullary fixation and arthroplasty was 73 ± 6 years and 75 ± 6.5 years respectively. Average delay in surgery for group A (PFN) and group B (hemiarthroplasty) was 5.7 days and 6.56 days, mean duration of surgery was 75 min (range 45 to 125) and 95 min (range 70 to 132), mean blood loss was 180ml (range 150 to 280) and 270 ml (range 250 to 420) respectively. Harris hip score at one year were better in arthroplasty group but almost comparable at two year.
Conclusion: Primary arthroplasty provides a stable, painless and reasonably functional joint, which provided early mobility and rehabilitation and hence is a better way of managing an osteoporotic unstable intertrochanteric fracture in elders especially. However, overall long term functional outcomes are almost similar for two groups.
Keywords: Intertrochanteric fracture, Internal fixation, Arthroplasty, Harris Hip Score
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Orthopaedics Surgery, Jawahar Lal Nehru Medical College Aligarh Muslim University, Aligarh, Uttar Pradesh, India. Email: |
Sabir A, Mohan R, Faizan M, Jilani L, Ahmed S, Shaan Z, Is It Worthy To Replace Hip Than To Go For Intramedullary Osteosynthesis In Unstable Intertrochantric Fractures In Elderly- A Prospective Comparative Study. ojmpc. 2020;26(1):19-23. Available From https://ojmpc.com/index.php/ojmpc/article/view/99 |