Systematic review of nerve injury following total hip replacement with posterior or lateral approach
Battacharjee D1*, Gandavaram S2, Singhai S3, Guduri V4, Kattimani R5, Dojode C6
1* Dhritiman Battacharjee, Specialist, Dept of Orthopaedics, Glan Clwyd Hospital, Bodelwyddan, Rhyl Wales, United Kingdom.
2 S Gandavaram, Dept of Orthopaedics, Glan Clwyd Hospital, Bodelwyddan, Rhyl Wales, United Kingdom.
3 S Singhai, Dept of Orthopaedics, Glan Clwyd Hospital, Bodelwyddan, Rhyl Wales, United Kingdom.
4 V Guduri, Dept of Orthopaedics, Glan Clwyd Hospital, Bodelwyddan, Rhyl Wales, United Kingdom.
5 R Kattimani, Dept of Orthopaedics, Glan Clwyd Hospital, Bodelwyddan, Rhyl Wales, United Kingdom.
6 C Dojode, Dept of Orthopaedics, Glan Clwyd Hospital, Bodelwyddan, Rhyl Wales, United Kingdom.
Background: Total hip replacement, is common surgical procedure, performed through posterior or lateral approach but it is yet not clear which method is safe and provides reduced risk of nerve injury. Nerve injury after total hip replacement can be severely debilitating leading to poor outcomes. Thus we performed this systematic review with the aim to assess the risk of nerve injury after THR by different surgical approaches and to evaluate the adverse effects and the functional outcomes of nerve injury after THR
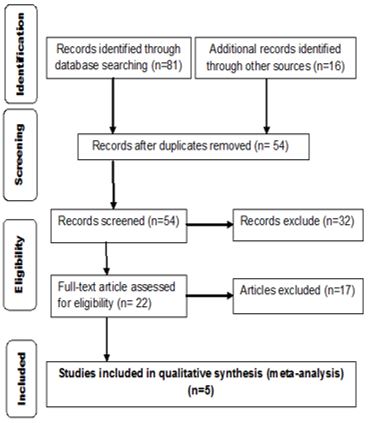
Material and Methods: A thorough literature search was conducted of Cochrane Bone Joint and Muscle Trauma Group, Cochrane Database of the Systematic Reviews, Cochrane Central Register of Control Trials, MEDILINE, EMBASE and CINAHL from their inception to 29 May 2014. Grey literature was located via the website www.opengrey.eu, conference proceedings and trial registries. Prospective and retrospective case series and case control studies were included in the systematic review. The inclusion criteria were adult population of 18 years and above with total hip replacement for osteoarthritis, dysplastic hip, acetabular fracture or revision total hip replacement. The exclusion criteria were patients below 18 years of age, with pre-operative nerve palsy or with previous medical conditions like stroke and low back pain. Cadaveric and biomechanical studies and studies conducted in non-English languages were excluded. Authors independently selected the studies using inclusion and exclusion criteria, assessed risk of bias and extracted the data.
Results: A case control study, two prospective case series and two retrospective case series were included in this systematic review. The studies selected overall reported 97 patients with nerve injury following 36735 total hip replacements (prevalence 0.2%). Only one out of the five selected studies reported, stated statistically significant effect of outcome of nerve injury after THR, following posterior approach compared to lateral approach.
Conclusion: The systematic review results revealed an overall very low quality of evidence and could not offer support for any particular surgical approach to reduce nerve injury during total hip replacement. The systematic review underlined the need for further studies to properly establish the risk factors associated with different surgical approaches to improve evidence based knowledge and reduce patient disability.
Keywords: Systematic, injury, posterior
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Specialist, Dept of Orthopaedics, Glan Clwyd Hospital, Bodelwyddan, Rhyl Wales, United Kingdom. Email: |
Battacharjee D, Gandavaram S, Singhai S, Guduri V, Kattimani R, Dojode C, Systematic review of nerve injury following total hip replacement with posterior or lateral approach. ojmpc. 2019;25(02):51-58. Available From https://ojmpc.com/index.php/ojmpc/article/view/83 |