Introduction
Unrecognized foreign bodies are focus for infection and when they are deep seated they can result in tendinitis, granuloma, deep infection and even osteomyelitis. Most common foreign bodies are wood, metal, plastic or glass [1]. Foreign bodies of circumferential nature like rubber band, animal hair, cloth, thread etc are tied on the forearm or wrist quiet commonly in India [2]. When these circumferential foreign bodies are left for prolonged period or are forgotten after applying, they can migrate and cause serious constriction bands, ulcers, discharging sinus and compartment syndrome [3].
On involvement of further deeper tissue and bones these circumferential foreign bodies can result in osteomyelitis involving typically ulna on ulnar surface and radius on radial surface only, seen as erosion of ulna and radius on medial and lateral surfaces only respectively. We report successful treatment by early surgical exploration, of such a case of rubber band tied on the wrist of a child and was forgotten, which migrated deep into the bones causing typical patterned osteomyelitis of both radius and ulna.
The purpose of reporting this case is to create general awareness regarding complications of such foreign bodies among surgeons to consider for prompt surgical exploration on visualizing the typical signature patterned lesion of the bone involving the outer surfaces of the bones only for foreign body removal.
Case report
A 4 year’s female child presented to our tertiary centre with pain, swelling and discharging sinus on an old circumferential scar at left wrist joint from 6 months. The pain was localized to the left wrist and hand, was moderate to severe and was associated with swelling at the wrist joint. She had fever on and off which was low grade.
On history, her parents denied remembering any history of trauma to left wrist. She had taken treatment by a doctor at a local clinic, regularly for past 6 months with analgesics and antibiotics, but the complaints did not improve. On inspection, there was circumferential healed scar mark at the wrist along with three discharging sinuses at the dorsolateral, dorsomedial and one on ventral aspect of the wrist on the scar itself.
There was history of continuous pus discharge from the sinus tract for the past 5 months, which was although scanty, but did not subside even after antibiotics treatment given by a local surgeon (Figure 1).
Figure 1: Pre op clinical photographs volar view (a) & dorsal view (b) showing circumferential healed scar mark at wrist along with three discharging sinus.

On palpation the wrist was warm and tender. The movements of the wrist and fingers were grossly restricted and there was no active extension of finger, although some flexion of fingers was present. Passive movements were very painful. Distal pulsations were palpable for both radial and ulnar arteries. Sensory supply of the hand was normal except for diffuse hyperalgesia over palm. Colour Doppler of the left upper limb showed normal vascularity. Hematological examination showed leukocytosis with WBC count of 16000/mm3, sedimentation rate was 39 mm and C reactive protein was 3.5 mg/l.
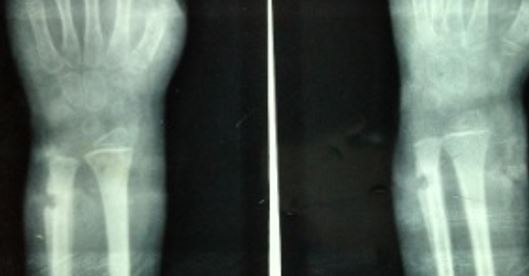
Patient was having 1 month old previous x-rays of wrist with her, which revealed a small lytic lesion of the ulna more on the ulnar side, along with the periosteal reaction but the radius seemed normal (Figure 2). Fresh x-rays were done, which showed osteomyelitis of both distal ulna and radius, with periosteal reaction and lytic lesion at both distal radius and distal ulna particularly on medial side of ulna and lateral side of radius (Figure 3).
Figure 2: 1 months old previous x-rays of wrist AP (a) & oblique (b) views showing small lytic lesion of the ulna particular on the ulnar side, along with the periosteal reaction but normal radius.
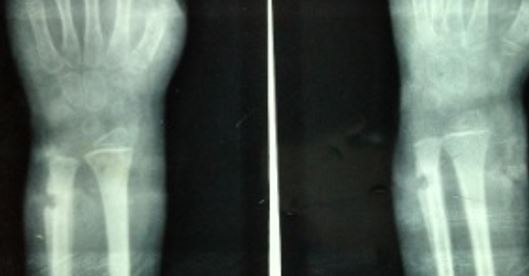
Figure 3: AP (a) & lateral (b) X-rays at presentation showing osteomyelitis of both distal ulna & radius, with periosteal reaction and lytic lesion on medial side of ulna and radial side of radius.

On visualization, of this typical signature pattern osteomyelitis causing lesion on ulnar surface of ulna and radial surface of radius, we suspected some circumferential foreign body inside and we decided to explore the wrist immediately. Under tourniquet control and under general anesthesia, we explored the wrist via circumferential incision excising the sinus tracts and the previous scar completely.