Objective Evaluation Of Tendon Morphology By Ultrasonography In Treatment Of Recalcitrant Tennis Elbow By Autologous Platelet Rich Plasma
Jain S1*, Banodha L2, Kelkar R3, Gautam V4
1* Saurabh Jain, Assistant Professor, Department of Orthopaedics, Mahatma Gandhi Memorial Medical College and Maharaja Yashwantrao Hospital, Indore, Madhya Pradesh, India.
2 L Banodha, Department of Orthopaedics, Mahatma Gandhi Memorial Medical College and Maharaja Yashwantrao Hospital, Indore, Madhya Pradesh, India.
3 R Kelkar, Department of Orthopaedics, Mahatma Gandhi Memorial Medical College and Maharaja Yashwantrao Hospital, Indore, Madhya Pradesh, India.
4 V Gautam, Department of Orthopaedics, Mahatma Gandhi Memorial Medical College and Maharaja Yashwantrao Hospital, Indore, Madhya Pradesh, India.
Background: Traditional therapies of tennis elbow have shown inconsistent outcomes as they do not deal with poor tendon healing properties secondary to poor vascularization. Local platelet rich plasma injections, which provide locally high concentration of growth factors, have shown its efficacy in treatment of tennis elbow on a subjective basis only.
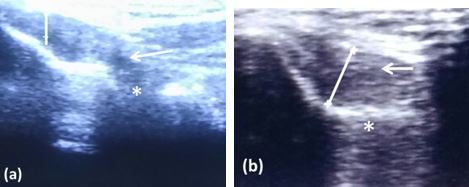
Material and methods: We tried to measure the efficacy of locally injected autologous PRP, subjectively by functional oxford elbow score and pain score as well as objectively by ultrasonographic evaluation of the morphologic changes (focal hypoechoic, odema, tendon thickness, fraying, tear, cortical erosion, calcification) in common extensor origin in 30 patients with mean age of 39.3 years of recalcitrant tennis elbow.
Results: The mean pain VAS Score improved from 7.7 before injection to 1.8 at final follow up i.e. after 6 months post injection. The Oxford elbow score improved from a mean of 19.2 prior to treatment to 41.3 after the injection at final follow up. 6 months post injection ultrasonography of the involved elbow showed decrease in focal hypoechoic, decreased edema, and improvement in thickness of the tendon and healing of the tear at the origin site.
Conclusion: This study confirms that local PRP by supplying growth factors helps to enhance the stromal and mesenchymal stem cell proliferation and increases tendon vascularity and prevents angiofibroblastic degeneration and thus improves tendon repair and healing property by releasing growth factors and increasing vascularity, which can be documented by improved tendon morphology.
Keywords: Tennis elbow, Platelet rich plasma, Ultrasonography
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Orthopaedics, Mahatma Gandhi Memorial Medical College and Maharaja Yashwantrao Hospital, Indore, Madhya Pradesh, India. Email: |
Jain S, Banodha L, Kelkar R, Gautam V, Objective Evaluation Of Tendon Morphology By Ultrasonography In Treatment Of Recalcitrant Tennis Elbow By Autologous Platelet Rich Plasma. ojmpc. 2019;25(1):23-29. Available From https://ojmpc.com/index.php/ojmpc/article/view/73 |