Hypovitaminosis D In Elderly Patients Presenting With Fractures
Shan Z1, Alvi Y2*, Ahmad S3, Jilani L4, Faizan M5, Asif N6
1 ZH Shan, Department of Orthopaedics, Jawaharlal Nehru Medical College and Hospital Aligarh Muslim University AMU, Aligarh, UP, India.
2* Yasir Alvi, Senior Resident, Department of Orthopaedics, Jawaharlal Nehru Medical College and Hospital Aligarh Muslim University AMU, Aligarh, UP, India.
3 S Ahmad, Department of Orthopaedics, Jawaharlal Nehru Medical College and Hospital Aligarh Muslim University AMU, Aligarh, UP, India.
4 LZ Jilani, Department of Orthopaedics, Jawaharlal Nehru Medical College and Hospital Aligarh Muslim University AMU, Aligarh, UP, India.
5 M Faizan, Department of Orthopaedics, Jawaharlal Nehru Medical College and Hospital Aligarh Muslim University AMU, Aligarh, UP, India.
6 N Asif, Department of Orthopaedics, Jawaharlal Nehru Medical College and Hospital Aligarh Muslim University AMU, Aligarh, UP, India.
Background: Vitamin D deficiency is seen in all races, age groups and ethnic backgrounds. It is estimated to affect more than one billion people worldwide. This study was done to find out vitamin D levels and its associated factors among elderly patients presenting with fractures.
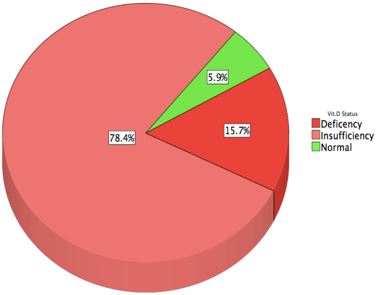
Material and method: This cross-sectional study was performed at our tertiary care hospital, in patients above 45 years, presenting with fracture as a result of trivial trauma. In all patients serum 25(OH)D level was measured. A level of serum 25(OH)D < 10 ng/ml was labeled as the deficiency, between 10 to 29 ng/ml as insufficient and ≥ 30 ng/ml as sufficient.
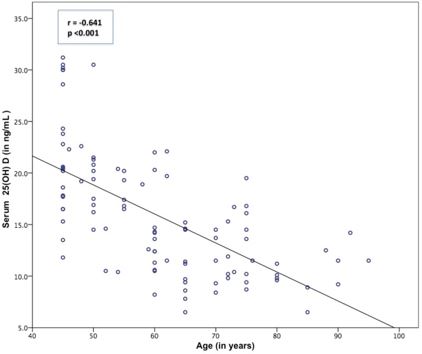
Results: A total of 102 patients were included in our study with mean age of 60.8 ± 13.4 years, out of which 60 were males and 42 females. Mean serum 25(OH)D level in our study population was 15.82 ± 5.88 ng/ml. We found 94.1% of the patients were having a low level of serum 25(OH)D i.e. less than 30 ng/ml, with 78.4% insufficient (between 10 to 29 ng/ml) and 15.6% deficient levels (below 10 ng/ml). Higher age, female, menopause and lack of sunlight exposure were found to be significantly associated with lower vitamin D levels.
Conclusion: This study gives us important inside of a high prevalence of hypovitaminosis D in elderly patients. Detection and prompt intervention of vitamin D deficiency at an early stage can be helpful in decreasing the fracture in these elderly.
Keywords: Vitamin D deficiency, Serum 25(OH)D, Hypovitaminosis D, Ageing
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Senior Resident, Department of Orthopaedics, Jawaharlal Nehru Medical College and Hospital Aligarh Muslim University AMU, Aligarh, UP, India. Email: |
Shan Z, Alvi Y, Ahmad S, Jilani L, Faizan M, Asif N, Hypovitaminosis D In Elderly Patients Presenting With Fractures. ojmpc. 2019;25(1):17-22. Available From https://ojmpc.com/index.php/ojmpc/article/view/72 |