Introduction
Heterotopic ossification (ectopic ossification), can be defined as the formation of mature lamellar bone at sites, where normally no ossifications occurs, like muscles and soft tissues [1]. The lesion comprises of fibroblasts and osteoblasts, with a high proliferating potential. It is quiet commonly seen in active young adults, especially among male athletes [2]. Trauma, either acute or chronic is a major cause leading to HO, and lesions adjacent to joints can be seen in some conditions with neurological component. Upon presentation, ossification becomes so extensive that it becomes evident and radiological studies reveal the benign behavior of the lesion.
Connective tissues like involuntary muscles, tendons, fascial sheaths, and ligaments are
the sites commonly involved in ectopic bone formation [3]. The flexor of the arm, the hamstrings and quadriceps femoris are the muscles, commonly involved in heterotrophic ossification (HO) [4]. The most common location of the heterotrophic ossification is represented by the pelvic ring, followed by the elbow, shoulder, and knee. Joint stiffness is often the pathognomonic characteristic of this disabling disease [5].
Synonyms for Heterotrophic ossification are myositis ossificans, florid ossification, ectopic ossification, neurogenic ossifying fibro myopathy [6, 7]. The histology of the lesions varies from osteoid osteoma - like features to osteosarcoma-like appearances [2, 8].
We report a case of traumatic heterotrophic ossification of quadriceps femoris, which was successfully managed with surgical resection, and continuous physiotherapy.
Case Report
A case of 26 year old male who, presented in our outpatient department with complaints of generalised swelling in right distal thigh, mild pain, restricted movement in right knee joint and difficulty in walking for 6 months. There was a history of road traffic accident 8 months back sustaining open injury over the right knee following which, he was diagnosed to have undisplaced unicortical fracture of anterior cortex of distal femur. Patient was managed elsewhere with debridement and primary wound coverage. The wound got infected after 10 days, for which repeated debridement with curettage was done. The wound got healed after a month, but patient was left with severe knee stiffness and difficulties in activities of daily living. The patient was then advised physiotherapy on regular basis, but there was no improvement in knee stiffness. The patient then went to a local therapist for massage therapy, but the problem got worsened.
Clinical examination revealed a generalized firm swelling noted in the anterior aspect of right distal thigh extending up to the knee. Overlying skin was non pinchable and puckered. Skin was adhered to underlying bone at one point. Range of motion (ROM) at knee was 0-10° with a normal ROM at hip (figure 1).
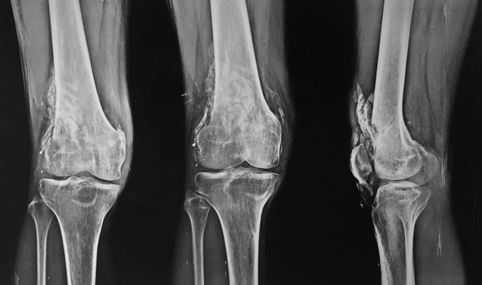
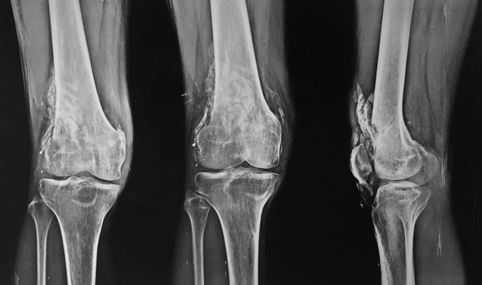
Patient was on continuous physiotherapy for 6 months, but had no improvement. X-rays revealed a well ossified mass anterior to anterior cortex of the right distal femur with some lateral extension, with a radiolucent cleft separating the ossified mass from cortex (figure 2).
Figure 1:

Figure 2:
As conservative measures produced no improvement in the patient, hence, surgical excision of the lesion was planned. Surgical resection of the ectopic ossified mass was done using a standard anterior approach to the knee joint. A well-defined mass (5cmX3cmX3cm) was excised from within the substance of rectus femoris posteriorly and mass on the lateral aspect of vastus lateralis was nibbled. Only easily resectable mass, was excised without causing much damage to overlying and underlying muscles. The adhesions were released from over the quadriceps and under the patella. Intra operatively knee flexion of 90 degrees was obtained after mass excision as shown in Figure 3.
Figure 3: