Introduction
Periprosthetic femoral fracture is a difficult surgical problem for orthopedic surgeons. It can happen during or after the operation. The ever-expanding indications for total hip arthroplasty are leading to more implants being placed in younger as well as in older patients with high functional demand. Also, prolonged life expectancy is contributing to an overall increment of periprosthetic femoral fractures. The incidence of periprosthetic femoral fractures (PFFs) has been reported to be between 1% and 11% over a primary and up to 18% over a revised hip femoral stem (1). Management of these injuries is often resource intensive and can present significant socioeconomic challenges. Understanding the principles of surgical management these cases and recognising when fixation or replacement is required is critical (2). Risk Factors for periprosthetic femoral fractures are osteoporosis, poor bone stock, uncemented femoral stem, revision of a femoral stem, previous fracture neck of femur treated by THR, osteolysis and aseptic loosening. These fractures can occur during previous implant removal, bone preparation and placement of the revision implant. History and physical examination reveal acute onset of pain, deformity and history of a fall. PFFs occurring over a THA can be divided into intra-operative and post-operative PFFs. Intra-operative fractures are estimated to occur in less than 1% of cemented and in 5.4% of uncemented primary THA, while in revision surgery the incidence of PFFs is higher, up to 3.6% during cemented and 20.9% during uncemented procedures. (7)
In general, in the context of a well-fixed femoral stem (Vancouver B1 or C) it is possible to retain the prosthesis and treat with internal fixation methods (8). When there is concern of loosening or instability around the stem (Vancouver B2, B3) then the literature supports revision arthroplasty surgery with or without internal fixation (9).
Radiographic Evaluation is done by full-length views of the femur (AP, lateral view), AP pelvic radiograph. Judet views are done to evaluate the floor, roof, and columns of the acetabulum. CT and MRI are done to rule out unusual complexity, especially around the acetabulum. Evaluation is done to exclude the possibility of infection by Inflammatory markers and intraoperative testing is done by frozen section analysis of periprosthetic tissue. Classification of periprosthetic femoral fracture is Vancouver classification. This system is based on site of the fracture, stability of the stem and quality of bone.
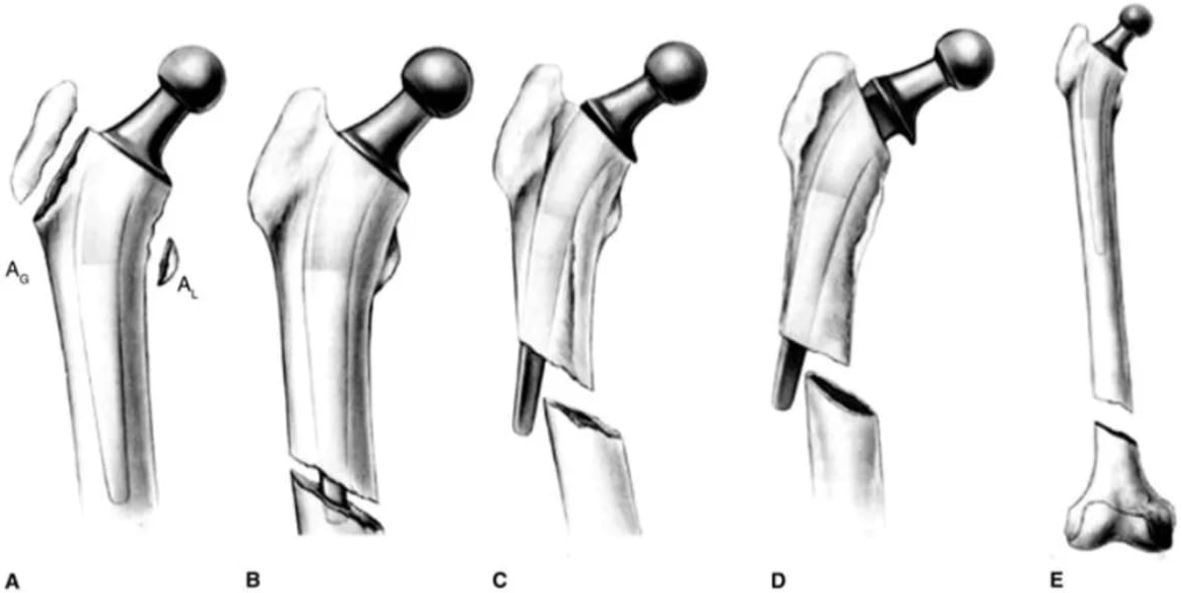
Type A fractures involve the greater or lesser trochanter, type B are diaphyseal starting around the stem and may extend distally whereas type C fractures are distal to the stem in the femoral shaft. The Vancouver system remains the most commonly used due to its simplicity and its application to surgical management.
Modified Vancouver Classification of Post-operative PFFs
A Proximal metaphysis
AG Around the greater trochanter
AL Around the lesser trochanter
B Bed of implant
B1 Stable stem
B2 Loose stem, good bone stock
Burst Highly comminuted fracture, more frequent in cemented stem
Clamshell* Displaced fracture of the medial cortex including residual neck, calcar and the lesser trochanter, more frequent in uncemented stem
Reverse clamshell Displaced fracture of lateral cortex with a “reverse obliquity” pattern
Spiral More frequent in cemented stem, loose bone-cement and/or cement-stem interface
B3 Loose stem, poor bone stock
C Clear of the implant, well below the prosthesis
D Clear of the implant, dividing 2 implants, a hip and a knee arthroplasty
There always remains some controversies surrounding the optimal management of peri-prosthetic fractures such as which internal fixation method is optimal in Vancouver B1 fracture and identification of stable or unstable stems when considering retention of the prosthesis (7).
Fixation option in the context of a vancouver B1 or C fracture are limited by restricted bony fixation proximally given the presence of a femoral stem and often in compromised bone stock. The use of single plate fixation for treatment of vancouver B and C type fracture with an overall failure of 33.9 %, high failure rates and need for reoperation have previously been described by Lindahl et al. The only plate is not a good choice for fixation because of high failure rate.
Cerclage wire or cable fixation is commonly employed in the management of intra-operative periprosthetic fracture at time of primary surgery however this technique may also be applied to management of post operative fracture. Cable-only fixation showed high failure rate and need revision surgery so only cable is not a good choice for fixation. A recent study demonstrated better outcome using the hybrid technique of cables and plate fixation around the stem.


