Introduction
Avascular necrosis of femoral head occurs due to impaired blood supply to the head of femur. It can be caused by fractures, dislocations, chronic steroid use, chronic alcohol use, coagulopathy, congenital causes and many other factors. But most common cause is Idiopathic. (1-4) The use of a non-vascularized bone graft is more attractive in treating the early stages of avascular necrosis of femoral head than vascularized graft because, it is significantly less technically demanding. (5,6)
Non-vascularized autologous bone grafting has several theoretical advantages. this method leads to the decompression of the avascular lesion and the elimination of the necrotic bone, breaking the cycle of ischemia and intraosseous hypertension in addition to providing growth factors from the graft [7].
The regenerative properties due to the presence of osteoblasts in the trabecular bone and the ability to procure a large amount of graft make the iliac crest the gold standard site of cancellous bone graft harvesting. [8,9] core decompression can be considered an effective treatment modality in the early stages (up to stage 2b) of AVN of the femoral head [10].
Therefore, this study was conceptualized to study the effect of core decompression along with cancellous bone grafting on cases of AVN of the femoral head.
Material and method
This prospective, interventional study was conducted in Global hospital, Ujjain from jan-2022 to march-2023. We studied 20 hips having early AVN of the femoral head treated by core decompression and autologous cancellous bone grafting with a graft taken from the iliac crest. AVN of femoral head (up to grade 2b of Ficat and Arlet classification) who met the inclusion and exclusion criteria are included in this study.
Inclusion criteria was patients with avascular necrocis of the femoral head up to stage 2b (Ficat and Arlet), patients aged between 18 and 60 years and patients giving consent for the surgical procedure and participation in the study.
Exclusion criteria was patients with previous infection of the hip Joint, neuromuscular disorder of the hip joint and severe osteoporosis.
AVN stage was confirmed preoperatively using an X-ray of the pelvis with both hip joints and an MRI of both hips. A preoperative workup was done. After taking written and informed consent, patients were taken for the operation theatre.
Patients were placed on a traction table in a supine position. Sterile painting and draping were done. Subsequently, a 2-3 cm mid- lateral longitudinal incision was made over the subtrochanteric region.The tensor fascia lata was split in the direction of its fibers, and the vastus lateralis muscle was elevated.
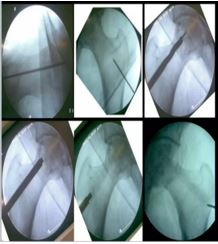
Under C-arm guidance, a 3.2 mm threaded guide pin was inserted through the lateral cortex into the affected part of the femoral head, with the entry point between the lesser trochanter and greater trochanter. The guide pin was directed toward the centre of the necrotic area of the femoral head. The guide pin was over-reamed with an 8 mm reamer. The cancellous bone graft was taken from the outer table of the iliac crest of the patient. The gap created with the cancellous bone graft was packed. Both the operative sites were washed thoroughly with normal saline and layer-wise closure was done with vicryl and ethilon. Finally, sterile dressing was done.
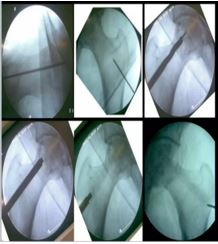
Figure 1: Core decompression of femoral head & bone grafting
Post operative management-Intravenous (IV) antibiotics were given till the third postoperative day, followed by oral antibiotics until suture removal. Dressing was done on the first, third, and fifth postoperative days. Physiotherapy started on day one which included knee mobilization, static quadriceps exercises, ankle pump, and toe movement. After one-week, partial weight bearing was started. Follow-up was done at 1.5 months, three months, and, finally, six months. Patients were assessed using the Harris Hip Score (HHS) and Visual Analog Scale (VAS) scores at follow-up.
Results
In our study, the majority (50%) of patients were in the 20-30-year age group, making it the most common age group, followed by the 31- 40-year age group (40%).There was a male predominance, with 17 out of 20 patients being male. All patients became symptomatic within the last year (range = 2-12 months). Of 20 patients, 11 presented to us within three months of developing symptoms (Table 1). Out of 20 patients, 10 were able to sit cross-legged, squat, and climb stairs without any significant problems.