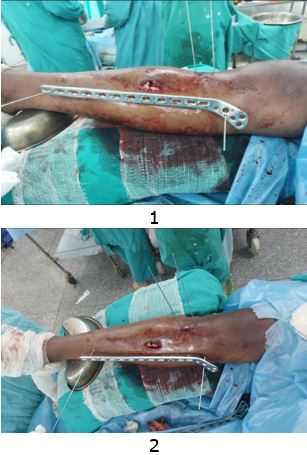
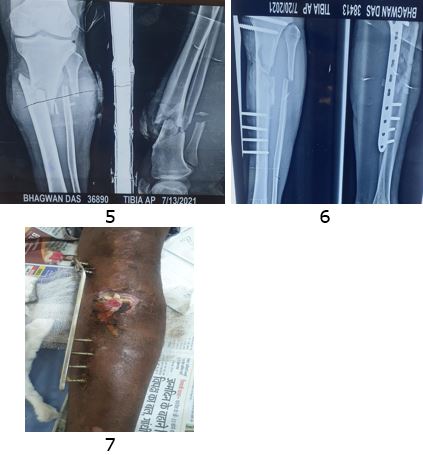
Supracutaneous LCP as a definite fixation method in compound metaphyseal and intraarticular fractures of tibia
Bajoria RS1*
1* R S Bajoria, Professor, Department of Orthopedics, Gajra Raja Medical College, Gwalior, Mp, India.
Introduction: Open fractures of distal and proximal tibia are common injuries encountered by orthopedic surgeons. Metaphyseal compound fractures are not suitable for ORIF with greater chances of infection, soft tissue complications and risk of plate exposure. With external fixator, treatment & fracture healing period usually increased & complication rates are quite high, so we managed these fractures by supracutenous LCP as external fixator; and results evaluated. We find out it a better alternative method to conventional external fixator. We evaluated the feasibility of supracutenous LCP as definite fixation methods in open fractures.
Material and methods: This study conducted from April 2020 to October 2023. Total 30 cases were included in this study. Open GA II & IIIA of tibia metaphyseal fractures in 18 cases and intra articular tibia fractures in 12 cases included in this study. Debridement & LCP plates fixation was done in external fixator manner. Proximal & distal tibia LCP fixed with long screws. Most fixations were done within 1 - 5 days of trauma. Patients were followed up till bony union. Minimum follow up was 6 months.
Results: 8 cases united in 4 months, 8 cases united in 6 months, 9 cases united in 6-9 months and 5 cases went in non-union. Average duration of union was 5.6 months. Functional outcomes evaluated by AKSS score for proximal fractures & by AOFAS for distal fractures. 15 cases have shown excellent results; with union, 11 cases have shown good results; soft tissues reconstruction required, 4 cases had bad results; due to infection. Overall, 26 cases were had good to excellent results.
Conclusion: We observed that external fixation in open fractures usually results in infection, delayed or non-union, requirement of further surgeries. Supracutaneous LCP as primary definite fixation can give excellent results in terms of stable & rigid fixation, early fracture union, less chances of second surgery, cost effective and better patient compliance & better functional outcomes.
Keywords: Supracutaneous LCP, definite fixation, compound fractures of tibia
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Professor, Department of Orthopedics, Gajra Raja Medical College, Gwalior, Mp, India. Email: |
Bajoria RS, Supracutaneous LCP as a definite fixation method in compound metaphyseal and intraarticular fractures of tibia. ojmpc. 2023;29(2):44-47. Available From https://ojmpc.com/index.php/ojmpc/article/view/177 |