A Prospective Analysis of Functional Outcome of Surgical Stabilization of Distal End Radius fractures with Plate Osteosynthesis.
Barua VK1*, Sirsikar A2, Naik S3, Sharma T4
1* Vinay Kumar Barua, Department of Orthopaedics, Netaji Subhash Chandra Bose Medical College, Jabalpur, M P, India.
2 A Sirsikar, Department of Orthopaedics, Netaji Subhash Chandra Bose Medical College.
3 S Naik, Department of Orthopaedics, Netaji Subhash Chandra Bose Medical College.
4 T Sharma, Department of Orthopaedics, Netaji Subhash Chandra Bose Medical College.
Introduction: Distal radius fractures (DRF) are the most common fractures of the upper extremities and due to population explosion, with an ageing society & enormous increase of high-speed motor vehicle accidents, the number of distal radial fractures can be expected to increase in the coming decades. Plate osteosynthesis has become the standard treatment for comminuted intra articular DRF. Main aim of this study was to analyse the functional outcome in patients stabilized by plate osteosynthesis with minimum follow up of 6 months.
Material and Methods: A prospective study was done on 46 patients with distal radius fractures who were operated with plate osteosynthesis, type of plate was decided as per fracture pattern and followed up at 1, 3, and 6 months and outcomes measured using Modified Mayo score, Grip strength tested by Dynamometer.
Observations: Volar plating was done in 34 patients; dual plating was done in 4 patients dorsal column plating was done in 8 patients. Average time of radiological union of fracture was 10 weeks, average time of clinical union of fractures was 8 weeks, average time to return to normal activity was 3 weeks, average time to return to professional activity was 4 weeks.
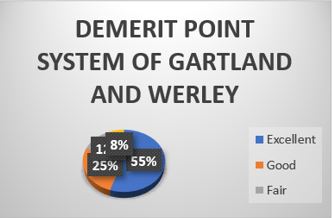
Results: According to Modified MAYO score 18 patients had excellent results, 10 had good results, 8 had fair and 4 had poor results. Grip strength was >80% compared to normal side in 29 patients, >60% in 8 patients and, <60% compared to normal side in 3 patients measured with a Dynamometer at 6 months.
Conclusion: Fractures of distal end radius managed with plate osteosynthesis is a good treatment modality with excellent results provided the surgeon has a sound knowledge of literature and a good surgical hand.
Keywords: distal end radius, plate osteosynthesis
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , , Department of Orthopaedics, Netaji Subhash Chandra Bose Medical College, Jabalpur, M P, India. Email: |
Barua VK, Sirsikar A, Naik S, Sharma T, A Prospective Analysis of Functional Outcome of Surgical Stabilization of Distal End Radius fractures with Plate Osteosynthesis.. ojmpc. 2022;28(2):51-59. Available From https://ojmpc.com/index.php/ojmpc/article/view/157 |