Paediatric Tuberculous spinal abscess causing compression at the lumbar level
Mehta R1*, Agrawal A2, Singh V3
1* Rahul Mehta, Associate Professor, Department of Orthopaedics, RD Gardi Medical College, Ujjain, Madhya Pradesh, India.
2 A Agrawal, Department of Orthopaedics, RD Gardi Medical College, Ujjain, Madhya Pradesh, India.
3 V Singh, Department of Orthopaedics, RD Gardi Medical College, Ujjain, Madhya Pradesh, India.
Incidence of paediatric spinal tuberculosis (TB) is increasing. Paediatric spinal TB is known to cause rapid bony destruction and deformity progression. We present a 4-year child with lumbar kyphotic deformity, progressive lower limb weakness and early bladder involvement. Imaging revealed near complete destruction and retropulsion of L4 vertebra with spine at risk signs. Posterior decompression, L1 to S1 fixation with pedicle screws and punching the remaining L4 body ventrally was performed. With aggressive post-operative physiotherapy and AKT patient recovered neurologically from Frankel C to Frankel E grade with complete radiological resolution of disease at final follow-up of 1 year. No further progression of deformity was observed at final follow-up.
Conclusion: Early diagnosis, timely and judicious surgical intervention is the key to management of paediatric spinal TB.
Keywords: Early diagnosis,timely and judicious surgical intervention is the key to management of paediatric spinal TB
| Corresponding Author |
How to Cite this Article |
To Browse |
Rahul Mehta, Associate Professor, Department of Orthopaedics, RD Gardi Medical College, Ujjain, Madhya Pradesh, India.
Email:  |
Mehta R, Agrawal A, Singh V, Paediatric Tuberculous spinal abscess causing compression at the lumbar level. ojmpc. 2022;28(1):48-49.
Available From
https://ojmpc.com/index.php/ojmpc/article/view/155 |
 |
Introduction
The incidence of vertebral TB is increasing and it accounts for 10-20% of all extra-pulmonary cases of TB(1). Thoraco-lumbar junction is the most commonly involved site followed by lumbar and cervical region.(2) Spinal TB occurs most commonly in children and young adults(3). Early diagnosis and intervention is required in children as it may lead to bony destruction, deformity of the growing spine and severe neurological complications.
Case Report
A 4yr old female child presented with the complains progressively increasing back pain and bilateral lower limb weakness since 2-3 months, with inability walk or sit without support since last 15 days. Frequency of micturition was increased and constitutional symptoms were present. Neurological status was Frankel grade C.(4)
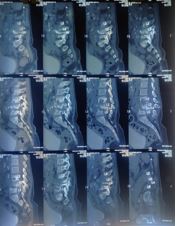
Pre-op xray suggested of mild lumbar kyphosis with vertebral destruction at multiple levels. MRI and CT scans revealed complete destruction with retropulsion of L4 vertebral body and partial destruction of L2L3L5 vertebra. Spine at risk signs were present hence surgery planned.
Surgical Procedure
Under GA in prone position with all bony prominences well padded. The procedure was performed under C-arm guidance. Midline skin incision given, posterior only approach was used. L3 partial L4 complete Lt. laminectomy with L1-S1 posterior decompression with instrumented fixation (3.5mm pedicle screws)was performed.
| Manuscript Received |
Review Round 1 |
Review Round 2 |
Review Round 3 |
Accepted |
| 2022-06-06 |
2022-06-12 |
2022-06-18 |
2022-06-24 |
2022-06-30 |
| Conflict of Interest |
Funding |
Ethical Approval |
Plagiarism X-checker |
Note |
| Authors state no conflict of interest. |
Non Funded. |
The conducted research is not related to either human or animals use. |
12.49 |
© 2022by Mehta R, Agrawal A, Singh Vand Published by Madhya Pradesh Orthopaedic Association. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License https://creativecommons.org/licenses/by-nc/4.0/ unported [CC BY NC 4.0].