Functional and radiological outcome of parallel plate technique in distal humerus fractures: a prospective study
Singh V1*, Bhinde S2, Patidar A3, Agrawal A4, Sharma S5
1* Vivek Singh, Professor, Department of Orthopaedics, R D Gardi Medical College and CRG Hospital and Associated Charitable Hospital, Ujjain, Mp, India.
2 S Bhinde, Department of Orthopaedics, R D Gardi Medical College and CRG Hospital and Associated Charitable Hospital, Ujjain, Mp, India.
3 A Patidar, Department of Orthopaedics, R D Gardi Medical College and CRG Hospital and Associated Charitable Hospital, Ujjain, Mp, India.
4 A Agrawal, Department of Orthopaedics, R D Gardi Medical College and CRG Hospital and Associated Charitable Hospital, Ujjain, Mp, India.
5 SK Sharma, Department of Orthopaedics, R D Gardi Medical College and CRG Hospital and Associated Charitable Hospital, Ujjain, Mp, India.
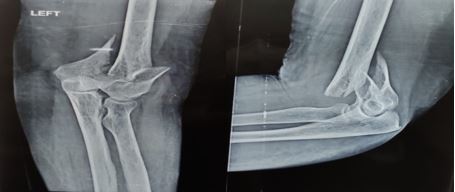
Background: Distal humerus fractures account for 2-6% of all fractures and 30% of all elbow fractures.These are difficult to treat because of their complex anatomy, metaphyseal comminution of fracture, subchondral bone and articular involvement with small fragments.
Aim: To study the results of intercondylar fracture distal end humerus treated with open reduction internal fixation with parallel plating technique in terms of final range of motion of elbow, union time and rate of complications.
Material and Methods: A total of 25 patients with distal humerus intercondylar fractures treated with parallel plating technique were included in this prospective randomised study. At each follow up patients were evaluated clinically and radiologically for union and outcomes were measured in terms of MAYO Elbow Performance Score(MEPS) consisting of pain intensity, range of motion, stability and function.
Results: Eight (32%) patients got excellent outcome, fourteen(56%) got good outcome and 3(12%) got poor outcomes and complications observed were infection, non union, hardware prominence and elbow stiffness.
Conclusion: Open reduction internal fixation(ORIF) with parallel plating technique can be a successful technique for fixation of distal humerus intercondylar fractures when its principles are strictly adhered to.
Keywords: Distal humerus fractures, parallel plating, MEPS score
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Professor, Department of Orthopaedics, R D Gardi Medical College and CRG Hospital and Associated Charitable Hospital, Ujjain, Mp, India. Email: |
Singh V, Bhinde S, Patidar A, Agrawal A, Sharma S, Functional and radiological outcome of parallel plate technique in distal humerus fractures: a prospective study. ojmpc. 2022;28(1):12-17. Available From https://ojmpc.com/index.php/ojmpc/article/view/153 |