Introduction
Coronavirus disease 2019 (COVID-19) originated in the city of Wuhan in Central China, and has spread quickly worldwide. It causes severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). At present, this newly identified disease is causing a large number of deaths and numerous confirmed cases worldwide and a major life risk to public health[1]. In February 2019 covid 19 was declared as public health emergency of international concern[2]. The cases started emerging from Europe and then to USA and now almost whole world is affected with it. Presently according to WHO, 162 million cases world-wide with 33 million confirmed deaths and around 222 countries are affected[3]. The disease is spreading across the world very quickly and lots of people around the world losing their precious lives.
India is country with population of 1.3 billion, second largest population after china. By the end of July 2019 there were 8 lac cases. Government of India implemented lockdown and compulsory social distancing to fight the disease all over the country to control the disease spread[4]. World Health Organization recommended doctor to population ratio of 1:1,000. India is still lacking adequet infrastructure in health sector in both public and private health sectors to fulfil the healthcare need of its growing population[5], and COVID 19 is putting a huge burden on it.
The first case of COVID 19 was reported in india on month of January 2020 in southern state of india.[6] India was quick to response to the spread of COVID 19 compare to other developed countries like United states, Italy, UK. The “Janata Curfew” was implemented by the prime minister of India in month of march with only 360 active cases. It was the world’s largest lockdown of 21 days, which failed to “flatten the curve” and second lockdown was initiated, which further underwent two more extensions. [7]
According to the data of health ministry of India on 20 may 2021, the total number of active cases were 26 million with 22 million recoveries. The national recovery rate was 86.74%. Total 20 million tests were done nationwide with mortality rate of 1.11%. Currently India has vaccinated over 180 million citizens.[15]
Standard Orthopaedic practice during pandemic
Orthopaedic patients presenting to casualty and outpatient department during COVID 19 pandemic 1. Infection- septic arthritis and osteomyelitis, 2. trauma, 3. elective OA patients with severe symptoms, 4. severe backpain patients, 5. post-operative follow-up patients, 6. post-operative infected cases, 7. metabolic diseases and bone cancer patients.
Steps to manage orthopaedic patients:-
- Safety precautions
One of the major hurdle is to segregate COVID 19 infected patients from non-infected patients, doctors as well as staff. To create a safe environment, the patients who are arriving to casualty need to be kept in separate cubicle.
Every patient entering the hospital need to be scanned by thermal body temperature check and should be sanitised with hand sanitizer. All patient entering to the hospital should be mandated to wear a mask, preferably 3 layered mask or N95 mask. Attenders accompanying the patients need to be restricted to one attender per person.
All the doctors and staff working with patient must be ensure that they are asymptomatic and should be under go regular testing for COVID 19 RTPCR. The examination areas has to be cleaned frequently with 2% chlorhexidine or 1% hypochlorite solution including tables, stools, doors and door knobs.
- Examination in emergency room
Doctors and staffs working in casualty need to be equipped with a N95 mask, face shield, hand sanitizers and a pair of gloves. All the patients arriving in the casualty with orthopaedic complaint are mandated to wear compulsory mask during history taking and physical examination. A detailed history of contact with COVID patient and sign and symptoms of COVID infection should be checked in all patients before examination.
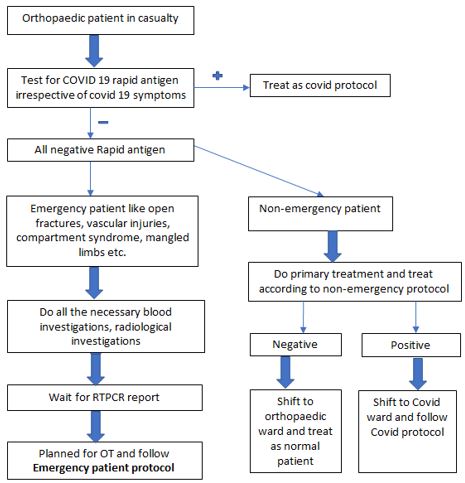
Compulsory use of PPE by health care provider in emergency department is one of the major protective measures to decrease the spread. All the patients who require admission should undergo screening test of RAPID COVID 19 test and are shifted to isolation ward with a negative report. Those patients are again tested for COVID 19 RTPCR, which takes 24hours on an average. After obtaining a negative RTPCR report, the patients are shifted to Orthopaedic ward and are managed accordingly. The patients with positive COVID report (either ANTIGEN or RTPCR) are directed to COVID hospital and managed accordingly.
- Treatment of OPD and elective patients
All the patients arriving to OPD must be symptom free and need to be checked for temperature. Mask need to be made compulsory for all individuals in OPD area. All the doctors and paramedical staffs should have a face shield. All health care provider should be instructed to follow social distancing and to use hand-sanitizer frequently also to use disposable gloves. All follow up post-operative patients should be segregated and are examined in a single room and instructed for home care if possible to avoid frequent visit.
All the elective patients with severe symptoms are examined and documented for their symptoms. Patients with low back pain, avascular necrosis, ankylosing hip, osteoarthritis and rheumatoid arthritis should be prescribed an adequate analgesia to delay and sort of surgical intervention. Bone tumour patients with pathological fracture, infection requiring admission should be investigated with all the routine tests, pre anaesthetic check-up, necessary consultation before operation. Proper history regarding COVID 19 contact, any sign and symptoms and symptomatic people in his family should be documented. RTPCR for COVID 19 for both patient and attendant must be done before admission. All the patient must be educated and stimulated for TELE-Medicine and to use electronic media for queries and follow ups.