Functional Outcome of Bilateral Total Hip Arthroplasty by Posterolateral Approach: A Prospective Study in Indian Population
Choudari P1*, Jain N2, Jain S3, Chauhan R4
1* Pradeep Choudari, Department of Orthopaedics, Sri Aurobindo Institute of Medical College and Post Graduate Institute, Indore, MP, India.
2 N Jain, Department of Orthopaedics, Sri Aurobindo Institute of Medical College and Post Graduate Institute, Indore, MP, India.
3 S Jain, Department of Orthopaedics, Sri Aurobindo Institute of Medical College and Post Graduate Institute, Indore, MP, India.
4 R Chauhan, Department of Orthopaedics, Sri Aurobindo Institute of Medical College and Post Graduate Institute, Indore, MP, India.
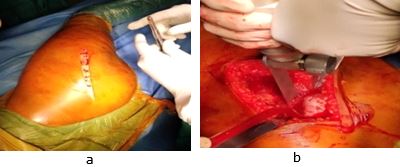
Background: Total hip arthroplasty (THA) is the most widely accepted surgical procedure for the treatment of Avascular necrosis of femoral head, with favourable clinical outcomes having been reported in various studies. Most patients that undergo THA suffer from primary osteoarthritis. The posterolateral (Moore’s) approach to hip permits easy access with fewer tissue dissection and blood loss while raising the risk of neural injury and postoperative dislocation of the prosthesis.
Material and Methods: This longitudinal study was conducted on 50 arthritic hips (25 patient) operated by a single surgeon with Bilateral THA via posterolateral approach (Southern Moore’s approach). All patients with bilateral osteoarthritis of hip secondary to avascular necrosis of hip (grade III or IV) more than 18 years of age, patients with normal septic profile and patients who were willing to undergo total hip arthroplasty according to our protocol were included in the study. The patients were followed up at the end of 6 weeks, 3 months and six months postoperatively after bilateral THA.
Results: Among 25 patients in this study, 20 patients (80%) were males and 5 patients (20%) were females. All the patients were between 18 to 60 years of age. The most common etiology for AVN was idiopathic in 11 patients (44%) followed by Steroid abuse in 8 patients (32%).The most common complication encountered in our study was Limb length discrepancy (LLD) in 3 patients (12%) followed by Posterior Dislocation of hip in 2 patients (8%). The mean pre op HHS was 28.22 and 26.73 for right and left hip which improved significantly post operatively with HHS of 82.36 after 6 months post operatively which suggest excellent improvement in clinical outcome.
Conclusion: Uncemented bilateral THA can be used in patients with excellent to good functional outcome at midterm follow-up, high satisfaction rate and lower rate of complications. Longer follow-up and multi-centric studies with larger sample size are necessary to establish confirmatory results.
Keywords: Arthroplasty, Hip, Bilateral, Avascular necrosis
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , , Department of Orthopaedics, Sri Aurobindo Institute of Medical College and Post Graduate Institute, Indore, MP, India. Email: |
Choudari P, Jain N, Jain S, Chauhan R, Functional Outcome of Bilateral Total Hip Arthroplasty by Posterolateral Approach: A Prospective Study in Indian Population. ojmpc. 2021;27(1):37-41. Available From https://ojmpc.com/index.php/ojmpc/article/view/132 |