Introduction
Conventional open posterior midline approach is the most common approach used for pedicle screws fixation for lower lumbar pathology. This approach requires excessive retraction of the bulky lower lumbar muscles, which results in paraspinal muscle damage and denervation, which may lead to postoperative flat back deformity and chronic back pain [1].
In order to prevent these complications, Wiltse in 1968, developed the paramedian approach, also known as posterolateral or paraspinal muscle sparing approach. It is based on lateral dissection between the muscles, two finger breadths away from the midline spinous process rather than midline approach elevating the muscles from spinous process, specifically used for the far lateral discectomy. This approach had advantages of minimal muscle injury, lesser intra-operative bleeding and a shorter hospital stay [2].
Later on, he modified his approach to the sacro-spinalis splitting approach to have clear cleavage between multifidus and longissimus paraspinal muscle [3]. In the process of further refinement, he extended the indications for the approach from lateral discectomy to other uses like insertion of pedicle screws and decompression of the opposite side from inside the vertebral canal [4].
We retrospectively evaluated the results of this modified Wiltse approach done for fixation of single level lumbar spinal instability as an alternative to conventional open posterior approach to avoid muscle damage and reduce radiation exposure.
Material and Methods
This retrospective study was conducted at our tertiary level institute from January 2017 to December 2019 in patients operated for single level lumbar spinal instability at L4-L5 or at L5-S1, via modified Wiltse approach.
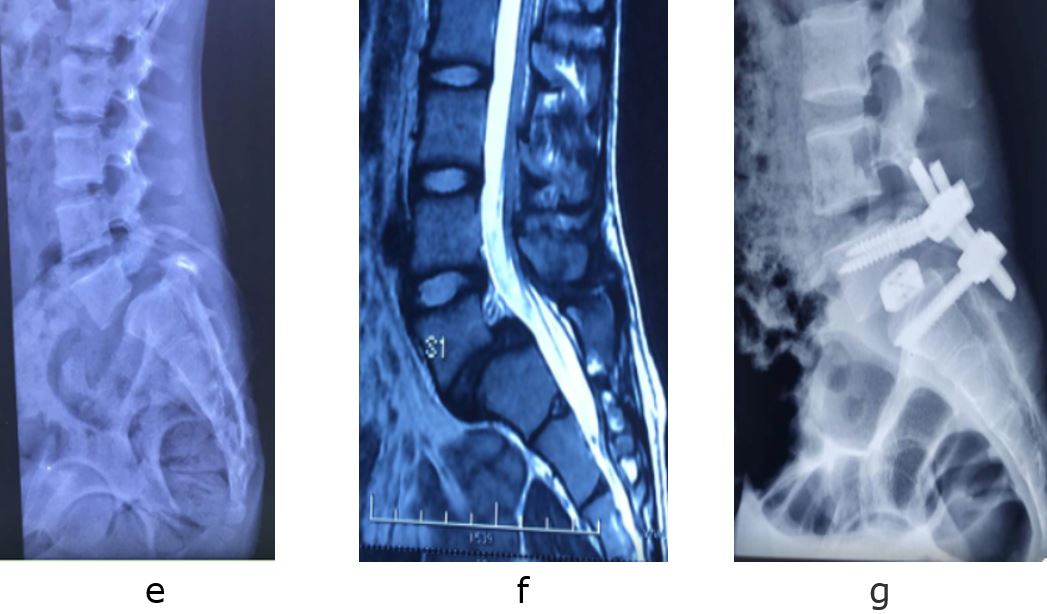
Institutional ethical clearance and written informed consent from all the patients was obtained. All patients with lumbar spine instability at L4-5 or L5-S1 operated via modified Wiltse approach with minimum one year follow up were included in the study. Lumbar spine instability was evaluated on dynamic X-ray’s and Magnetic resonance imaging. Burst fractures and spondylolisthesis either grade 1 or 2 at single level were included in the study.
Patients operated for more than grade 2 listhesis, for more than one level involvement of lower lumbar instability or for lumbar canal stenosis were excluded from study.
All the patients were operated under general anesthesia in prone position over longitudinal bolster under image intensifier. All patients were operated via modified Wiltse approach, via single midline skin incision. After midline skin incision and subcuticular dissection in midline, lumbosacral fascia was identified. Two paraspinal vertical incisions were made through the fascia approximately 3-4 cm lateral to the spinous process at the marked level on both the side.
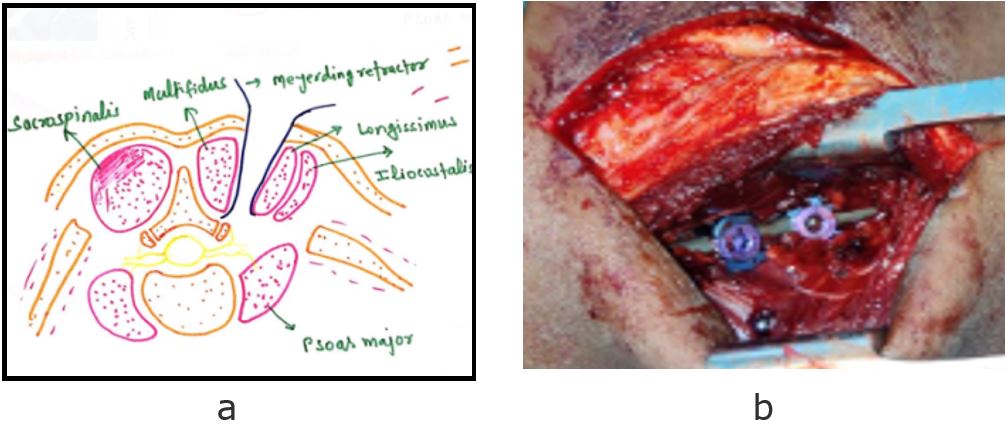
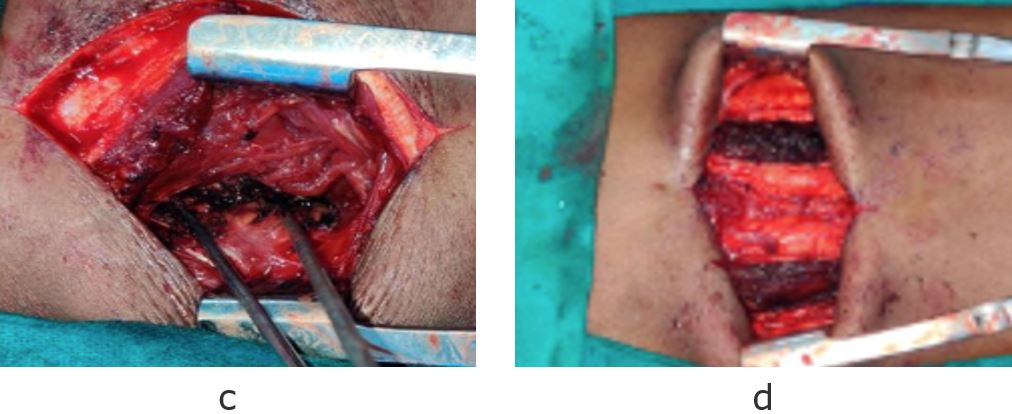
Superficial and deep fascia was split longitudinally along with blunt splitting of sacrospinalis, identifying the clear cleavage plane between the natural gap of multifidus medially and longissimus laterally (figure1). Small amount of fat helped to delineate this plane. The muscles were then meticulously teased apart in avascular plane till the transverse process. Following this the transverse process and facet joints were palpated and after retraction with Meyerding’s retractors, the entry point for the pedicle screws was identified at mamillary process.
Slightly nibbling the base of superior articular facets, the desired size pedicle screws were inserted into the appropriate vertebra after, inspecting the walls of the channel with a ball-tipped probe. The direction and position of pedicle screw placement was confirmed with fluoroscopy. For applying another pedicle screw, the retractor was moved up or down, maintaining it between the inter-muscular planes.
The required numbers of pedicle screws were inserted and then assembly was completed by placing connecting rods. In case, of spinal trauma only pedicles screws were inserted whereas in cases of spondylolisthesis, the facet joint was removed and bone filled inter body cage, was additionally inserted after discectomy and preparation of vertebral body endplates by high speed burr.
Local bone grafts were harvested from posterior iliac crest with same incision in case of L5 vertebral burst fracture for posterolateral fusion whereas in cases of listhesis bone graft removed during decompression and facet removed was used for inter body fusion. After checking decompression, fixation and reduction under image intensifier the closure was done with both sides of fascia with running suture without any drain.
Postoperatively, patients were mobilized with help of lumbar corset from second postoperative day and discharged after three to five days. Suture removal was done at two weeks. Patients were followed monthly for three months and then three monthly up to one year. All patients were assessed for pain by VAS score, neurology, blood loss, duration of surgery and hospital stay. Fixation of the pedicle screws was assessed radiologically.
Results
12 patients of single level lumbar spine instability at L4-L5 or L5-S1 were included in the study. The mean age in the group was 34.6 years (range 16 to 45 years). 4 patients were male and 8 were female. Out of 12 patients, 2 patients were with L5 vertebral body burst fracture, 6 patients had L4-5 and 4 patients had L5-S1 isthmic spondylolisthesis.
Mean blood loss for the surgery was 150 ml (range 134 to 170 ml). The average C arm exposure was 12.5 (range 8 to 21). The average length of hospital stay was 3.5 days. None of the patients had any postoperative neurological complications or deterioration. The mean VAS score improved from 8.3 pre-operatively to 3.3 at 3rd post-operative day and finally to 1.2 at one-year follow-up.