Neglected Cauda Equina Syndrome Due To Prolapsed Lumbar Intervertebral Disc In An Adolescent Patient: A Case Report And Review Of Literature
Gawande J1, Verma P2, Mishra S3, Lakhtakia P4
1 Jeetesh Gawande, Assistant Professor, Department of Orthopaedics, Shyam Shah Medical College, Rewa, MP, India.
2 PK Verma, Department of Orthopaedics, Shyam Shah Medical College, Rewa, MP, India.
3 S Mishra, Department of Orthopaedics, Shyam Shah Medical College, Rewa, MP, India.
4 PK Lakhtakia, Department of Orthopaedics, Shyam Shah Medical College, Rewa, MP, India.
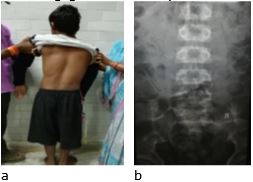
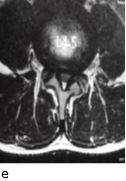
Case report: Lumbar disc herniation is very rare in children and adolescent age group. We report a rare case of two months old neglected case of post traumatic L4-L5 disc herniation causing cauda equina syndrome and bilateral foot drop in a 13-year-old patient. He was treated successfully with emergency L4 laminectomy and L4-L5 discectomy, and he recovered fully without any restricted activity. Cauda equina is a surgical emergency, which should be diagnosed and operated as early as possible for good results, even if the patient presents late.
Keywords: Cauda equine syndrome, Lumbar disc herniation, Laminectomy
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| Gawande J, Verma P, Mishra S, Lakhtakia P, Neglected Cauda Equina Syndrome Due To Prolapsed Lumbar Intervertebral Disc In An Adolescent Patient: A Case Report And Review Of Literature. ojmpc. 2021;27(1):46-49. Available From https://ojmpc.com/index.php/ojmpc/article/view/113 |