Introduction
Tarlov cyst is a perineural cyst, which was first described by Tarlov, after whom they are named. They are usually asymptomatic and are seen as an incidental finding at autopsy [1].Tarlov described first case of symptomatic perineural cyst and recommended its removal. Very few cases of such Tarlov cyst are reported in the literature [2-4].
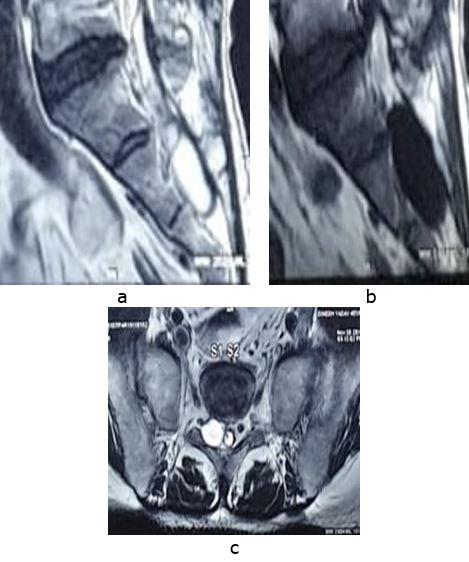
Most of the cysts are asymptomatic, but some of them can be symptomatic. The cyst can present as low back pain, sciatica, coccydynia or cauda equina syndrome, which when symptomatic, may require surgical treatment [4]. Diagnosis of cyst can be confirmed on MRI, which shows the fluid filled cystic lesion arising from the sacral nerve root near the dorsal root ganglion [5].
We here report such a rare case of symptomatic sacral Tarlov cyst presenting as back pain and radiculopathy which was successfully treated by surgical excision.
Case Report
A 45 year old male, labourer by occupation presented to outdoor patient department with history of insidious onset pain in lower back since 8 months.
There was no history of trauma, jerk or history of lifting any heavy object. The pain was localized to lower back, dull in nature with no diurnal or postural variations. Pain was initially relieved with rest and NSAIDS but had aggravated since last 2 months affecting the daily activities of the patient.
There was history of claudication and aggravation of pain on long standing. The pain had started radiating to left lower limb upto the ankle and toes. There was no history of bladder bowel dysfunction. The constitutional symptoms like loss of appetite, fever, weight loss or malaise were absent. He had no other complaint related to other body parts with bilateral hip and knees being normal.
On examination, there was mild local tenderness in the sacral area and lower back. Straight leg rising was 40º on left side and 80º on right side. There was weakness of ankle dorsiflexors, toe flexors and extensors (MRC grade 3) on left side with no sensory deficit. Right side was normal. All the reflexes were normal bilaterally.
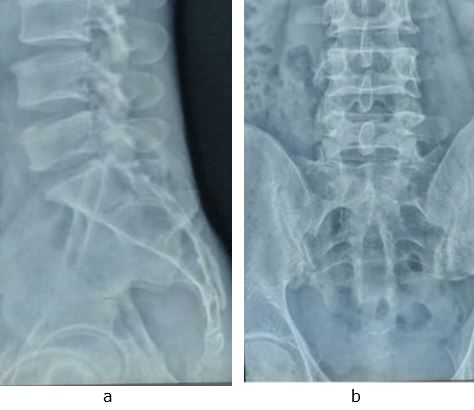
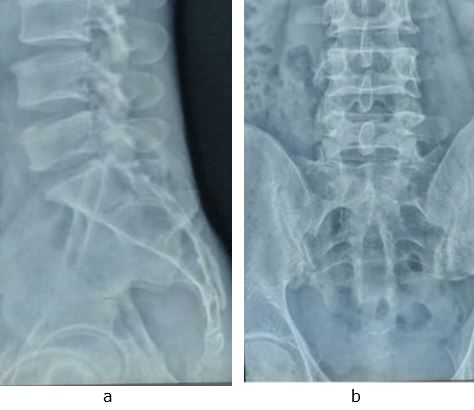
All haematological investigations and radiographs of lumbosacral spine were normal. MRI of the lumbosacral spine revealed a right sided extra dural, 3.8×1.8cm fluid filled cyst at level of S2 vertebra causing medial compression of dural sac.
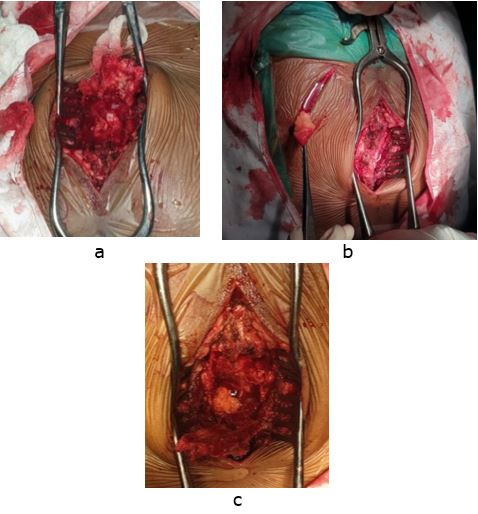
After routine pre-operative fitness patient was planned for surgical excision of cyst. Patient was operated under general anaesthesia in prone position via midline dorsal approach. Sacral laminotomy was done and a window was made in the sacrum. Flaps of ligamentum flavum elevated to expose the cyst (Figure 3a).
The cyst was excised and the dural sac was decompressed and a free fat graft taken from right gluteal region (Figure 3b) was placed over the after the plication of cyst wall.
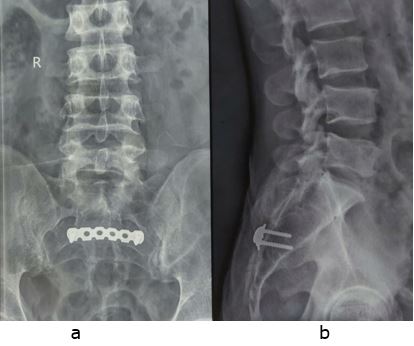
Finally osteosacral flap was reinforced using a Recon plate. The excised cyst was sent for histopathological examination which conformed presence of nerve cells in the cyst confirming the diagnosis of Tarlov cyst.
Figure 1:Lumbosacral X rays spine AP (a) and lateral (b) view with no obvious lesion
Post-operatively, there was no deterioration of neurology, and patient had immediate relief from radicular pain after the surgery. His motor power increased by grade one at 2 weeks of the surgery with no complains of the pain at back or radiculopathy. At 2 weeks post-surgery, he was able to walk without any claudication.
Discussion
Tarlov cysts are most commonly found in sacral region between perineurium and endoneurium of nerve root, although they can be present at any spinal segment. Small, asymptomatic Tarlov cysts are not uncommon and may be seen in 5 to 9% of the general population but large cysts that cause symptoms are relatively rare [2]. Cyst is common in females (86%) and in age group of 31 to 60 years (80%) [3]. Our case was a 45 years male who was labourer by profession.
Clinical presentation of the cyst can be variable. It can present with local or radicular pain, or different motor or sensory deficit, with or without involvement of bladder and bowel, depending on the size, location and relationship with the nerve root. Radicular symptoms from caudal nerve root may vary from sciatica, sacral or buttock pain, vaginal or penile paraesthesia or sensory changes over the buttocks, perineal area and lower extremity. Rare, but a larger cyst can even result in cauda equina syndrome [3,4].
Radiographs and CT scans are usually normal except for bone erosion of the spinal canal or neural foramina.