Giant cell tumor of proximal radius: A rare case report and review of literature
Jain T1, Bharadwaj L2, Tiwari DA3*, Verma R4
1 T Jain, Department of Orthopaedics, Gandhi Medical College, Bhopal, MP, India.
2 L Bharadwaj, Department of Orthopaedics, Gandhi Medical College, Bhopal, MP, India.
3* Dr Anurag Tiwari, Assistant Professor, Department of Orthopaedics, Gandhi Medical College, Bhopal, MP, India.
4 R Verma, Department of Orthopaedics, Gandhi Medical College, Bhopal, MP, India.
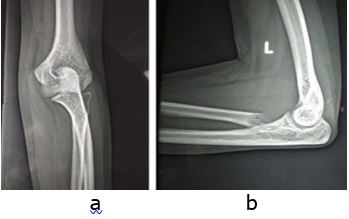
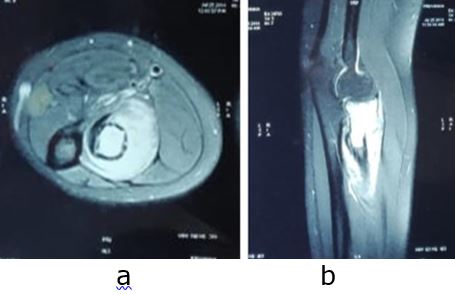
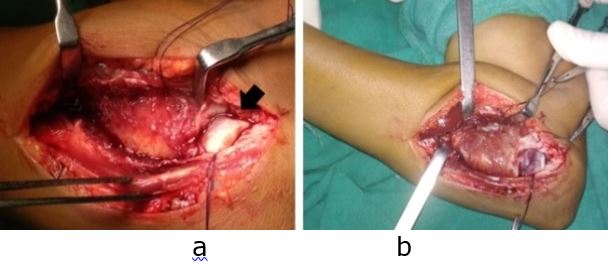
Case report: Giant-cell tumor (GCT) of the bone is benign bone tumor which usually arises from the epiphysis of long bones. Distal femur and proximal tibia are the most common sites of this tumor. The proximal radius is extremely rare site of this particular tumor. We present a rare case of Giant cell tumor of proximal radius in a twenty-one year old girl, for which wide margin resection was performed successfully with no recurrence, complications or disability seen at one year follow up.
Keywords: Giant cell tumor, proximal radius, resection
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Orthopaedics, Gandhi Medical College, Bhopal, MP, India. Email: |
Jain T, Bharadwaj L, Tiwari DA, Verma R, Giant cell tumor of proximal radius: A rare case report and review of literature. ojmpc. 2020;26(1):40-44. Available From https://ojmpc.com/index.php/ojmpc/article/view/103 |