Comparative Study between Minimally Invasive Percutaneous Plate Osteosynthesis and Open Reduction Internal Fixation For Management Of Proximal Humerus Fracture
Choudhari P1*, Verma A2, Jain N3
1* Pradeep Choudhari, Professor, Department of Orthopaedics, Shri Aurobindo Medical College, Indore, Madhya Pradesh, India.
2 A Verma, Department of Orthopaedics, Shri Aurobindo Medical College, Indore, Madhya Pradesh, India.
3 N Jain, Department of Orthopaedics, Shri Aurobindo Medical College, Indore, Madhya Pradesh, India.
Background: Fractures of the proximal humerus comprise nearly 4% of all fractures and 26% of fracture of humerus. Surgical options ranges from open reduction internal fixation (ORIF), intramedullary device fixation, external fixation to hemi arthroplasty. We compared the clinical and radiological outcomes of minimal invasive plate osteosynthesis (MIPO) and open reduction and internal fixation (ORIF) in patients with proximal humerus fractures.
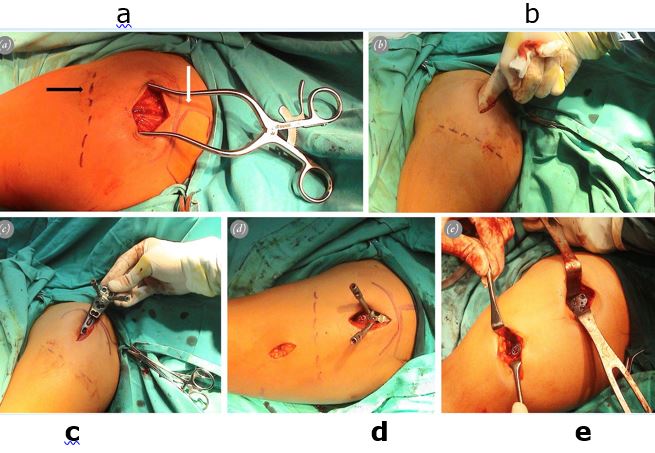
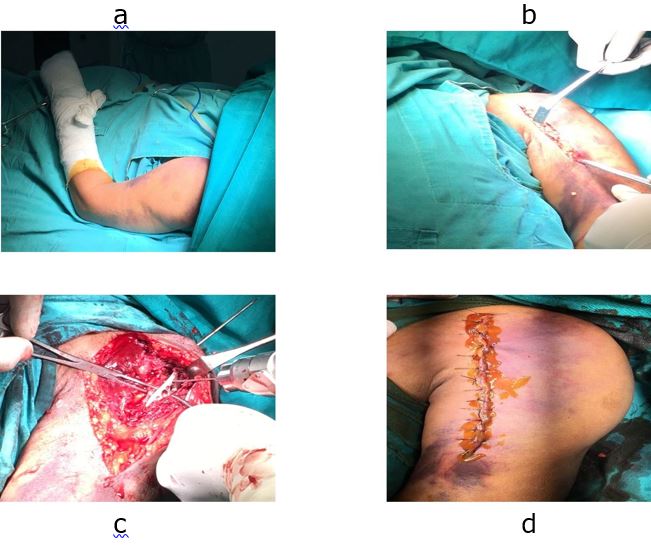
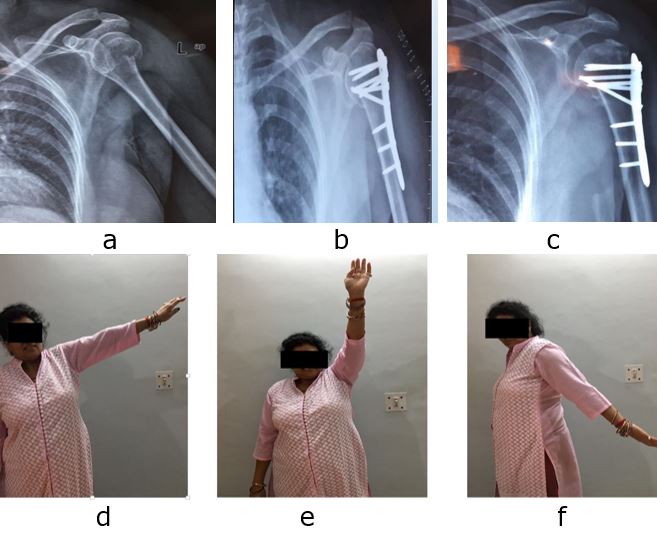
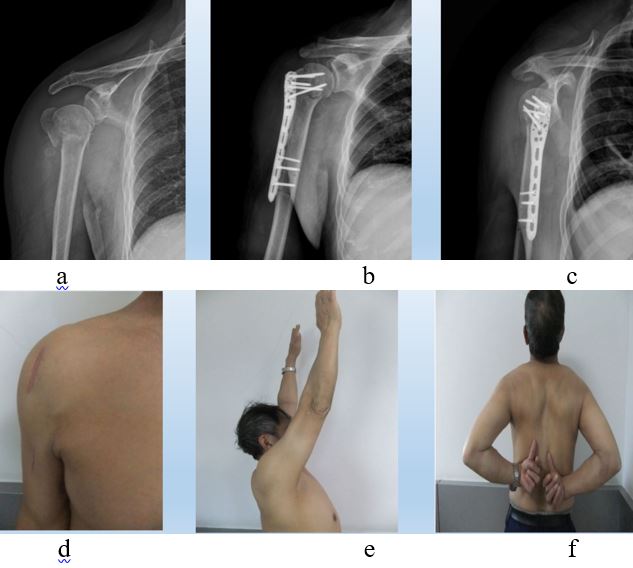
Material and Methods: This prospective study included 24 patients with 2 part and 3 part proximal humerus fracture treated with ORIF or MIPO technique, with 12 patients in each group. A matched pair analysis was performed and patients were followed up for 3 months, 6 months and 12 months both radiographically and clinically using Constant and Murley score.
Results: The average of patients was 47.2 years. Average blood loss and mean duration of surgery was 287.50 ml and 102.9 mins, in ORIF group and 198.33 ml and 93.75 mins in MIPO group. The mean Constant Murley Score at 12 months in the MIPO group was 77.00, while in the ORIF group it was 72.33. MIPO group experienced significantly less pain, higher satisfaction in activities of daily living, and greater range of motion. In the MIPO group, only one patient had infection whereas in ORIF group three patients, had complications with one each having infection, varus collapse and malunion
Conclusion: The use of MIPO with a locking compression plate in the management of proximal humerus fractures is a safe and superior option compared to ORIF.
Keywords: Proximal humerus, minimally invasive plate osteosynthesis (MIPO), locking compression plate
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Professor, Department of Orthopaedics, Shri Aurobindo Medical College, Indore, Madhya Pradesh, India. Email: |
Choudhari P, Verma A, Jain N, Comparative Study between Minimally Invasive Percutaneous Plate Osteosynthesis and Open Reduction Internal Fixation For Management Of Proximal Humerus Fracture. ojmpc. 2020;26(1):24-29. Available From https://ojmpc.com/index.php/ojmpc/article/view/100 |