Our case was also a case of 3 week old neglected case, which was due to the primary treatment done by bonesetter.Subtalar dislocations mostly occur in young adults after a high energy trauma such as a fall from height or road traffic accidents [4,5].
Various reports hypothesize mechanism of injury of posterior subtalar joint dislocation as forced hyper-plantar flexion of foot which leads to a progressive subtalar ligament weakening resulting in a complete tear of ligament if the plantar flexion force is prolonged [4-8]. Our case was also an active middle aged male with no comorbid condition sustaining injury due to fall from height with landing on dorsum of inverted and plantarflexed foot.
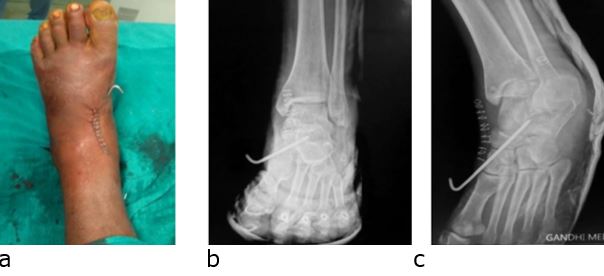
Diagnosis of posterior subtalar joint dislocation is easy with anterior-posterior and lateral radiographs. Inokuchi et al, defined the posterior subtalar dislocation on a lateral radiograph, when the head of the talus is seen perched on the posterior margin of the navicular and the posterior portion of the talus resting in the posterior subtalar facet of the calcaneum in the absence of any significant displacement or rotation of the foot in frontal view radiograph [5,9].
Recommended treatment to avoid further damage to skin, soft tissue, neurovascular structures and to reduce the chances of avascular necrosis of the talus, is prompt closed reduction as soon as possible under sedation or general anesthesia with constant counter-traction and flexion at knee so the gastrocnemius muscle is relaxed [6-9].
For reduction initially, the force is applied in the same direction as the existing deformity, then traction is applied, and at the same time a force in opposite direction of the dislocation is applied by a firm digital pressure over the head of the talus from anterior to posterior, passing through plantar flexion to dorsiflexion. The reduction is usually associated with an audible clunk [4,5,6-9]. Post reduction immobilization is done in non-weight bearing cast but the period of immobilization is controversial [10,11].
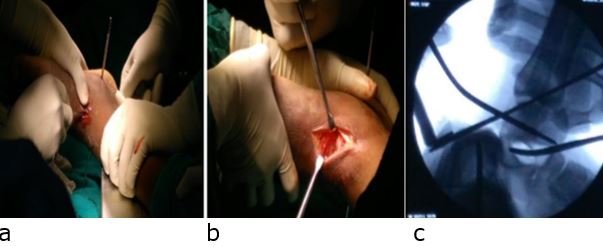
A delayed presentation, soft tissue interposition, interposed bony fragments, severe swelling or capsulo-ligamentous retraction renders the closed reduction difficult and which requires open reduction, which is required in 10 to 20% cases [12].
Since our case was also a 3 weeks neglected case with history of maltreatment and massage present, the closed reduction attempt failed and we could reduce it only after open reduction.
Conclusion
Posterior subtalar dislocations are extremely rare injuries which require early diagnosis, anatomical reduction, stable fixation of peritalar joint fractures, and the resection of small, free osteochondral fragments for the prevention of early posttraumatic arthrosis which, in turn, may cause pain, joint stiffness, and an unsatisfactory final result.
References
1. Judey P. Observation dune luxation metatarsienne. Bull Fac Med Paris. 1811;11:81–6. [Crossref][PubMed][Google Scholar]
2. Broca P. Memories sur les luxations sous-astragaliennes. Mem Soc Chir 1853;3:566–656. . [Crossref][PubMed][Google Scholar]
3. Malgaigne JF, Buerger CG. Die Knochenbrüche und Verrekungen. Rieger, Stuttgart, 1853. pp 820. [Crossref][PubMed][Google Scholar]
4. Prada-Cañizares A, Auñón-Martín I, Vilá Y Rico J, Pretell-Mazzini J. Subtalar dislocation: management and prognosis for an uncommon orthopaedic condition. Int Orthop. 2016;40(5):999-1007. [Crossref][PubMed][Google Scholar]
5. Inokuchi S, Hashimoto T, Usami N. Posterior subtalar dislocation: case report. J Trauma 1997;42(2):310–13. . [Crossref][PubMed][Google Scholar]
6. Bibbo C, Anderson RB, Davis WH. Injury characteristics and the clinical outcome of subtalar dislocations: a clinical and radiographic analysis of 25 cases. Foot Ankle Int. 2003;24(2):158–63. [Crossref][PubMed][Google Scholar]
7. Fortin PT, Kou JX. Commonly missed peritalar injuries. J Am Acad Orthop Surg. 2009;17(12):775–86. [Crossref][PubMed][Google Scholar]
8. Garofalo R, Moretti B, Ortolano V, Cariola P, Solarino G, Wettstein M, Mouhsine E. Peritalar dislocations: a retrospective study of 18 cases. J Foot Ankle Surg 2004;43(3):166–72. . [Crossref][PubMed][Google Scholar]
9. Siddiqui YS, Zahid M, Bin Sabir A et al. Neglected peritalar dislocation: a case report with review of literature. J Clin Diagn Res. 2011;5(4):849–52. [Crossref][PubMed][Google Scholar]
10. Bali K, Kumar V, Bhagwat K et al. Closed posterior subtalar dislocation without any associated fracture: a case report and review of the literature. Foot Ankle Surg. 2011;17(3):40–2. [Crossref][PubMed][Google Scholar]
11. Camarda L, Martorana U, D’Arienzo M. Posterior subtalar dislocation. Orthop. 2009;32(7):530. [Crossref][PubMed][Google Scholar]
12. Budd H, Wimhurst J, Davis B et al. Irreducible posterior subtalar dislocation with incarceration of a fracture of the anterior process of the calcaneum. J Bone Joint Surg Br. 2010;92(7):1025–7. [Crossref][PubMed][Google Scholar]
Disclaimer / Publisher's Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of Journals and/or the editor(s). Journals and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.