Introduction
Sprengel shoulder, which is characterized by congenital high riding scapula, is a rare complex deformity of shoulder griddle [1]. It is diagnosed as upward elevation of scapula in relation to thoracic cage or abnormally high placed scapula. Eulenberg, first described this condition of undescended scapula in 1863, and claimed its cause as traumatic dislocation of the scapula [2]. Later, it was Otto Sprengel who described the pathology and proposed a theory of its existence in 1891. The scapular embryonic primordium appears in 5th intrauterine week at the level of 4th to 5th cervical vertebrae & acquires its final morphology by 8th week of gestation & descends till 12th week over the upper 5 ribs to reach the correct anatomical position. This failure to descend leads to sprengel deformity [3].
The exact cause of the interruption of the normal caudal migration of the scapula during fetal development is unknown, but different theories have been postulated, like cerebrospinal fluid leak through the membranes of the roof of the fourth ventricle into the adjacent tissues of the neck, increased intrauterine pressure, and abnormal articulation of the scapula to the cervical vertebrae with abnormal muscle formation (fibrous, cartilaginous, or osseous omovertebral) [4].
Females are more affected and it is bilateral in about 10-30% with a predilection to left side. It can be part of other congenital anomaly. It is associated with severe cosmetic deformity and functional leads to limitation of shoulder movements [5]. We report such a rare case of isolated congenital sprengel shoulder with was treated by Green’s procedure successfully.
Case Report
A 6 year old male child visited to us in outdoor patient department with complains of visible deformity of left shoulder. The child was delivered by full term normal vaginal delivery. He had full immunization completed. Parent and child denied any other complain present, other than the deformity.
Familial history was unremarkable for any congenital disorder. On detailed history, the deformity and asymmetry of shoulder folds was observed by the parents at the age of one year of the child but they did not take any treatment. Gradually, the deformity is increasing and has grown to its current size which is not cosmetically accepted to the parents as well as the child.
There is also difficulty in dressing up himself as well as difficulty in carrying his school bag. Child would complain of pain in left shoulder after returning from school. On clinical examination, there was asymmetrical elevation of the left shoulder fold compared to the right side, which was visible both from front and back.
Since the deformity was severe, initial inspection gave impression of congenital short neck with torticollis as well, but careful examination after proper exposure showed no torticollis although slight deviation of head towards left side was noted. His neck and its movements were normal.
Inspection from back showed that inferior angle of both the scapula was at different level with left side higher up than right. Also the inferior angle of left scapula was medially displaced. Deformity was firm hard in consistency and mobile. Range of motion on left side, particularly, overhead abduction, external rotation and overhead elevation of shoulder was reduced grossly, compared to contralateral side and rest of the shoulder was normal. He had weakness pectoralis major muscle and serratus anterior muscle as seen as winging of the right scapula. Neurological examination as well as all other systemic examination was found to be absolutely normal.
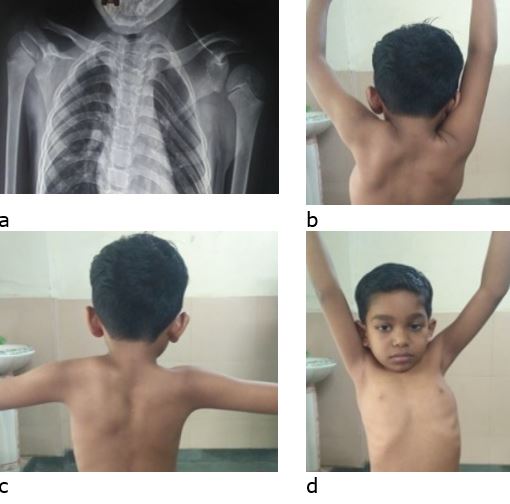
Routine radiographs were done including a chest radiograph PA view, axillary view and a scapular view. Radiographs showed high riding of the left scapula with superior angle of left scapula reaching almost level of C4 cervical spinal level (fig 1). Also the scapula was medially rotated and adducted. No abnormality was noted in left clavicle or head of humerus. Cervical rib or fusion of cervical vertebrae was absent.
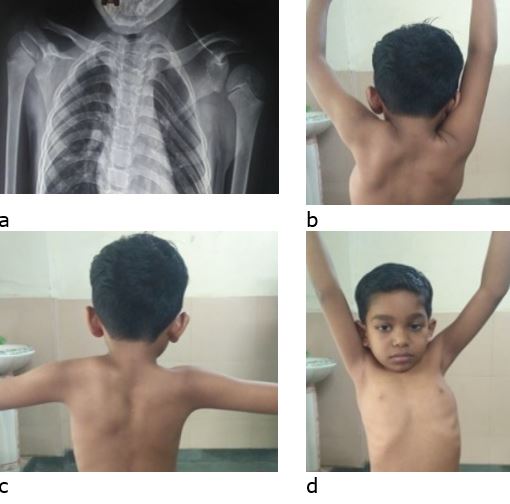
After routine haematological investigations and pre-anaesthetic work up patient was planned for scapulopexy by modified Green’s procedure. In general anaesthesia, in prone position the scapula was opened by dorsal midline approach extending from base of neck to inferior angle of scapula. Soft tissue dissected to undermine laterally toward the medial border of scapula. Lateral border of
trapezius was identified and was separated from underlying latissimus dorsi by blunt dissection. Using an osteotome trapezius is released from spine of scapula and retracted. Rhomboideus major and minor are released from their insertion at lateral border of scapula. Omovertebral bar was identified and resected, and contracted levator scapulae muscle was released from supraspinous part of the scapula.
Figure 1: Pre operative radiographs AP view (a) of chest and both shoulder showing high riding scapula on left side and clinical photographs (b to d) showing deformity & restricted movements.