Introduction
The recent advances in management of Spinal cord Injury (SCI) are based on evolving understanding of spinal mechanics, injury mechanics, improved instrumentation, better imaging modalities and better rehabilitative care. However management of thoracolumbar fractures remains controversial for many reasons. Firstly, to determine which injuries require operative treatment and which require non-operative treatment is difficult; secondly, to determine which is the best approach to be considered for the SCI when treated operatively; and lastly, to determine whether surgical management should have a direct decompression or if indirect decompression is sufficient [1].
Similarly there has never been a clear consensus regarding the effectiveness of decompression and fixation in spinal cord injury. Several authors like Roy Camille (1986), Cotler et al (1986), Transfeldt et al (1990), Anderson et al (1993) and Rahimi-Movaghar et al (2005) have opined that operative intervention has benefits like early mobilisation and rehabilitation thereby enhancing neurologic recovery [2-6]. Whereas several authors like Bohlman and Eismont (1981), Clark (1981) and Wood et al (2003) have opined that doing surgery has its own harmful effects on patients which outweigh the advantages [7-9].
Currently, the treatment of fractures of thoracolumbar spine is determined mainly by three factors which include, the morphology of the fracture, the neurology of a patient as it is an indicator of functional integrity of spinal cord, and which specific structures are injured [10]. Further till date, the role of decompression in patients with incomplete SCI is supported only by level III and limited level II evidence and there is no definite evidence to support the role of decompression in complete SCI [11].
Hence, in this study we attempt to look for the neurological recovery of patients with paraparesis due to traumatic incomplete thoracolumbar spinal cord injury treated by reduction, posterior stabilization and decompression.
Material and Methods
A total of 36 cases of incomplete spinal cord injury presented to our casualty department during the two years 2017 to 2018 were included in the study. Institutional ethical clearance and proper informed and written consent from all the patients was taken before the study.
All patients between age group 18 to 70 years with traumatic fracture involving thoracolumbar spine with incomplete neuro-deficit (American Spinal Injury Association (ASIA) Impairment grades B, C and D were included in the study. Patients with complete neuro-deficit (ASIA grade A), or pathological fracture were excluded from the study.
In all patients a detailed history and thorough examination was done evaluating pain, tenderness, motor examination, sensory and autonomic examination including assessment of bladder and bowel, etc.
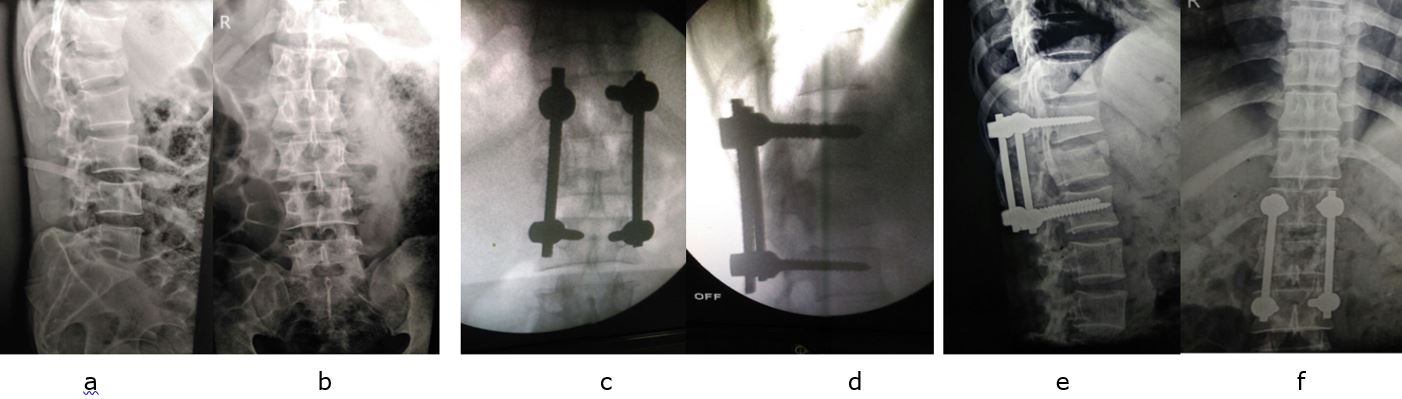
Initial ASIA grade was calculated according to American Spinal Injury Association (ASIA) Impairment and recorded and was revised daily. After routine investigation and fitness, all patients were operated under general anaesthesia in prone position over bolsters, using posterior midline approach to spine. After insertion of pedicle screws posterior decompression was performed using laminectomy and finally fixation and distraction with rods was done to achieve correction of deformity (fig. 1).
Rehabilitation was started pre-operatively unless contraindicated by other injuries. Patients were given appropriate nursing care, active and passive physiotherapy, DVT prevention centripetal massage, bowel care (using biological bulk forming agents like isabgol / psyllium husk, laxatives were given if required), skin care, air/water mattresses (in patients with sensory loss), chest physiotherapy and psychological support. Regular bladder irrigation was done with mild antiseptic solution when self-retaining catheter was there for unavoidable reasons. Regular follow ups were done and at each follow up ASIA grade was analysed and recorded. Patients completing follow up of minimum 6 months were only included in the study.
Statistical analysis was done using Statistical Package of Social Science (SPSS Version 22; Chicago Inc., USA). Chi-square test was used to determine significant differences. Significance level was fixed at 95% confidence interval (P < 0.05).
Results
A total 36 patients with incomplete spinal cord injury with mean age 33.7 years (range 18 to 60) were included in study, out of which 22 were males and 14 were females. The most common mode of injury was fall from height found in 58% cases followed by motor vehicle accidents found in 36% cases. The mean injury to surgery interval was 14 days (range 5 to 40 days). Initial neuro-deficit as per ASIA score was D in 18 cases (50%), 8 cases (22%) had grade B and 10 cases (28%) had grade C.
After a follow up of 6 months the neurological status of 24 cases (67%) improved by more than at least one grade and 3 cases had improvement by two grades with p value 0.001 (table 1). Complications were found in 9 patients (25%), which included bed sore (14%), urinary tract infection (5%), deep infection (3%) and chronic backache (3%). All the complications were treated symptomatically.
Discussion
Spinal trauma presenting with neuro-deficit can lead to gross morbidity and disability. In-spite of best treatment by decompression and fixation, the results of neurological recovery are inconsistent and unpredictable [12-13]. Jun et al (2011) showed 92 % improvement of at least one Frankel grade with an average of 1.7 grade improvement in thoracic and lumbar fractures treated using posterior decompression and fusion, whereas Lee et al reported only 53.6 % improvement [14,15].