Introduction
Total hip arthroplasty (THA) has evolved into a reliable and suitable surgical procedure to relieve pain and restore function among patients with damaged or degenerated hip joints [1-3]. Indication for a THA ranges from radiological evidence of joint damage, persistent pain, and/or functional disability that is not adequately relieved by non-surgical treatment to patients with primary osteoarthritis, fractures or rheumatoid arthritis [1,4-6].
The annual number of THA has risen steadily worldwide during the last decades. As the number of primary surgical interventions grows, the number of revisions is expected to increase [7]. The outcome of a successful THA depends on numerous factors other than the surgery itself.
The predictability of the outcomes of THR is excellent in the older age groups, whereas the longevity of the implant in young and active patients still remains unsatisfactory, with failure rates ranging from 20% to 42% [8-10]. We evaluated the outcome of all uncemented THA patients operated at our center to analysis our results and compare it with available literature.
Material and methods
A total of 180 hips were operated with total hip arthroplasty from January 2013 to August 2017 at our center. All patients with in age
group 20 to 70 years operated for uncemented THA who gave written informed consent were included in study. 30 hips were lost to follow up or did not give consent for the study and hence were excluded from the study, making the final cohort of 150 hips in our study.
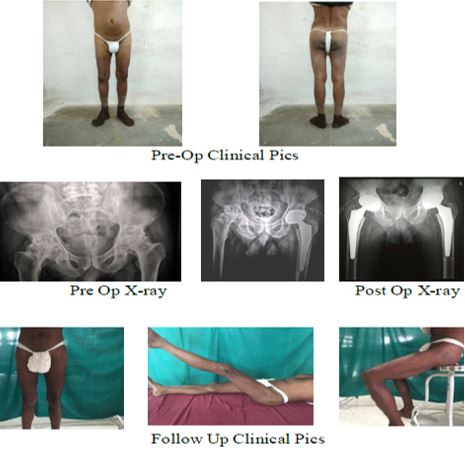
In all patients a detailed history and thorough examination was done evaluating pain, tenderness, deformity, gait, range of motion, limb length discrepancy, neurovascular status etc. Pre operatively Harris Hip Score and SF-36 Score was also recorded. All patients was subjected to routine blood investigation, Chest X-ray, ECG, X-ray pelvis with both hips and lateral view of involved limb and pre-anesthetic fitness before surgery. Patients were operated spinal or epidural anesthesia in floppy lateral position by surgeons of almost same experience and expertise (Figure 1).
Postoperatively, all patients were subject to same rehabilitation protocol like active quadriceps exercises, knee and ankle exercises from second post-operative day, weight bearing with support on third day post-operative day and suture removal on 14th day. Regular follow ups were done and at final follow up functional assessment was done, using Harris Hip score.
Statistical analysis was done using Statistical Package of Social Science (SPSS Version 22; Chicago Inc., USA). Quantitative variables were compared using mean values and qualitative variables using proportions. Significance level was fixed at P < 0.05.
Figure 1: Intraoperative photos showing position (a) acetabular (b) & femoral (c) implantation

Results
A total 150 hips in 115 patients were included in study out of which 89 were male and 26 were female. The mean age was 38 years (range 28 to 68 year). 88 % of our cases were less than 50 years and 62 % were less than even 40 years. 38 % of the cases have fixed deformity at the involved hip, among which fixed flexion deformity was commonest seen in 14% of cases. All the fixed deformities were corrected and none of the patients had fixed deformities postoperatively. The most common indication of THA was avascular necrosis of hip, seen in 66.7 % hips followed by rheumatoid and posttraumatic arthritis seen in 10 % each. The mean follow-up was 23 month (range 12 to 48 month)
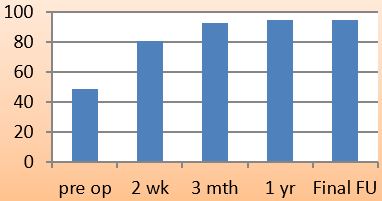
The mean pre-op Harris Hip Score of 49 (range 28 to 78) improved to 95.07 (range 87 to 98) postoperatively at final follow up. This improved Harris Hip Score was seen as continuous improvement from pre op to regular subsequent visits and at final follow-up which was statistically significant (p<0.05) (Figure 2). Mean SF-36 score was reduced from 78.90±6.71 (range 64 to 90) pre-operatively to 40.35±3.67 (range 31 to 49) at final follow up which was statistically significant (p<0.05) (Figure 3).
Figure 2: Mean Harris Hip score at follow-up visits