Comparative Study on Outcome of Early Aggressive and Standard Rehabilitation after Anterior Cruciate Ligament Reconstruction
Tantuway V1, Mustafa Johar SA2, Banerjee T3, Narware S4, Prajapati A5, Murtuza R6*
1 V Tantuway, Department of Orthopedics, Index Medical College Hospital and Research Centre, Indore, Madhya Pradesh, India.
2 S A Mustafa Johar, Department of Orthopedics, Index Medical College Hospital and Research Centre, Indore, Madhya Pradesh, India.
3 T Banerjee, Department of Orthopedics, Index Medical College Hospital and Research Centre, Indore, Madhya Pradesh, India.
4 S Narware, Department of Orthopedics, Index Medical College Hospital and Research Centre, Indore, Madhya Pradesh, India.
5 A Prajapati, Department of Orthopedics, Index Medical College Hospital and Research Centre, Indore, Madhya Pradesh, India.
6* R Murtuza, Department of Orthopaedics and Traumatology, Index Medical College Hospital and Research Centre, Indore, Madhya Pradesh, India.
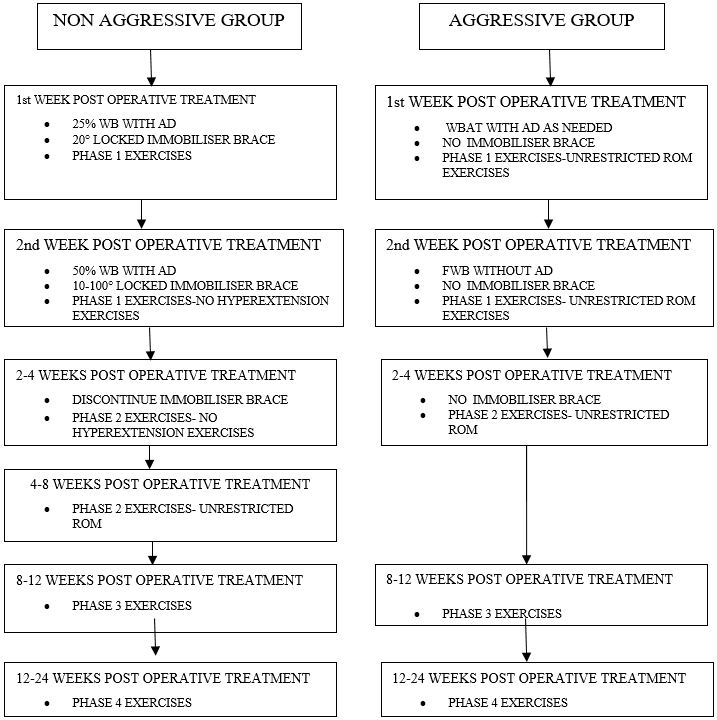
Background: Anterior cruciate ligament rupture is one of the most common debilitating knee injuries that can result in significant functional impairment. Although ACL reconstruction (ACL-R) is a commonly practiced surgical intervention, controversy still lingers with regard to graft selection and rehabilitation protocol, both of which are largely influenced by surgeon preference. The post-operative restrictions are largely based on the theory of graft and fixation vulnerability, with concerns related to compromising the biological healing process of the reconstructed graft during the first 12 weeks postoperatively. To date, controversy still lingers in evaluating the effects that aggressive rehabilitation has on clinical outcomes with semitendinosus graft. The aim of this study was to investigate whether immediate full weight bearing combined with aggressive rehabilitation in ACL-R significantly altered postoperative outcome over one year, relative to a program that included partial weight bearing and standard rehabilitation protocol in the immediate post-operative period.
Methods: The study was a prospective randomized clinical trial, with all patients being recruited by a single senior orthopedic surgeon at our institute after a confirmed diagnosis of an isolated ACL rupture by clinical examination and magnetic resonance imaging. Seventy patients were enrolled in the study from June 2015 to August 2017. Informed consent was taken. Clearance from ethical committee of the institute was taken. Patients were evaluated pre operatively and post operatively at the end of 1, 3, 6 months and 1 year for outcomes.
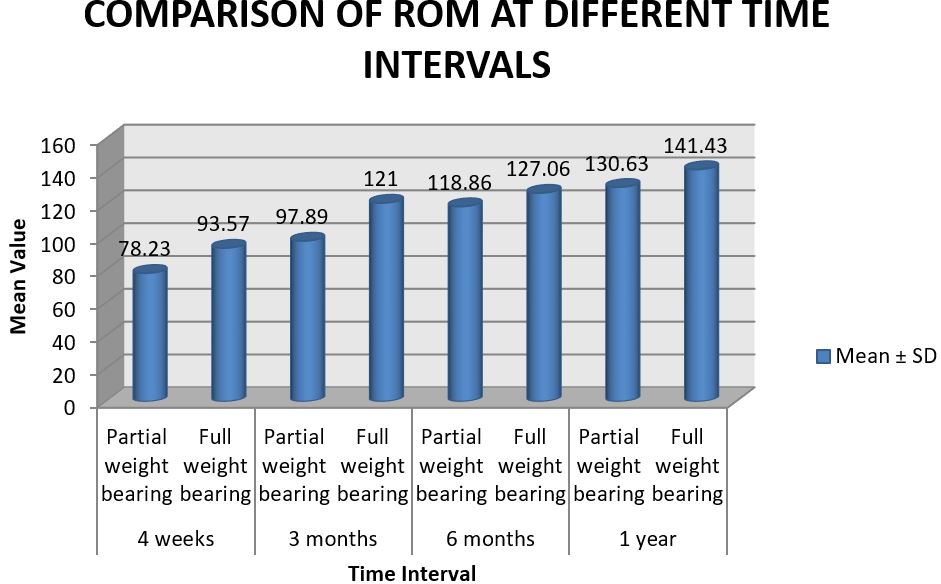
Results: In this prospective study conducted with seventy patients, we found better results in group 2 (full weight bearing) as compared to group 2 ( partial weight bearing) in terms of IKDC scoring, range of motion (ROM), ROM difference from opposite knee and fixed flexion deformity. The results were statistically significant.
Conclusion: We conclude that aggressive rehabilitation to be superior to standard rehabilitation after isolated ACL-R using STG .
Keywords: ACL, ACL-R, Rehabilitation
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , , Department of Orthopaedics and Traumatology, Index Medical College Hospital and Research Centre, Indore, Madhya Pradesh, India. Email: |
Tantuway V, Mustafa Johar SA, Banerjee T, Narware S, Prajapati A, Murtuza R, Comparative Study on Outcome of Early Aggressive and Standard Rehabilitation after Anterior Cruciate Ligament Reconstruction. ojmpc. 2018;24(1):25-35. Available From https://ojmpc.com/index.php/ojmpc/article/view/65 |