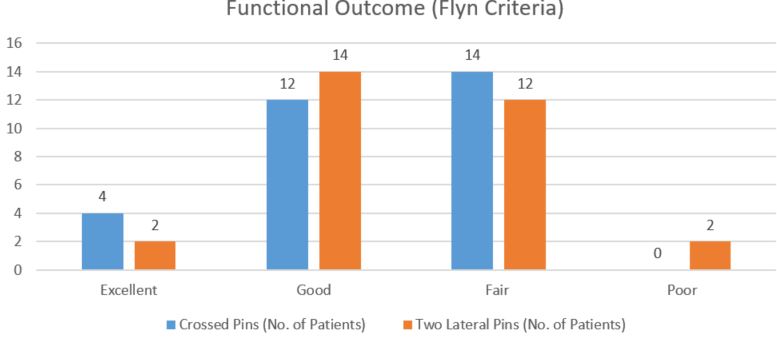
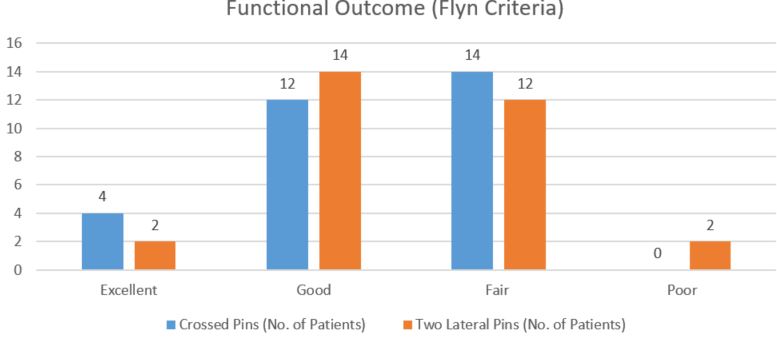
Figure 1: Functional Outcome of two groups
Mean carrying angle loss was 30 in lateral K wire group and 20 in cross K wire group, which was statistically significant(p<0.05).
This loss of carrying angle was more in lateral group probably due to less stable construct. Loss of range of motion was 10° in cross k wires group and 11° in lateral pinning group, which was not statistically significant. In this study, no pin tract infection was noted, no ulnar nerve was injured.
Loss of reduction was seen more in lateral wire group but eventually all achieved radiological union with < 5 angulation. The difference in functional outcome between the two groups was not statistically significant (P=0.69).
Discussion
Fracture that occurs at supracondylar area or metaphysis of distal humerus is labelled as Supracondylar Fracture. For closed reduction and percutaneous pinning, two configuration of K-wires exists either lateral pinning or cross K-wires. In this study, the average age was 7 years (range 2-12 years) with peak incidence in 5-8 years. Other authors reported similar age groups, average age 7 years by Ramsey and Griz [6], 6.4 years by Nacht et al [7].
In this study, there were 90% male, Fowles and Kassab reported 89% [8] and Nacht et al 50% male preponderance [7].
In this study, left sided fractures were more than right sided fractures. Fowles and Kassab showed left (57%) more involved than right [8]. Similar results were seen in study by Nacht et al (55%) [7].
In this study, fall on outstretched hand (96%) was the most common mode of injury, similar findings were shown by Mostafavi and Bhuyan [9,10].
In our study, the average radiological union was seen in 5 weeks (range 3 to 9 weeks). Sudheendra et al reported average radiological union at 7.6 weeks [4] Rijal and Pandey reported radiological union in 6 weeks [11].
In our study, Cross k wires had better stability. Lee SS et al and Zioutset al reported that medial and lateral entry provides greater torsional rigidity than lateral entry pin fixation does [12,13]. Sudheendra et al. in their study noted 82% excellent results and 18% good results in cross k wires case and 71% excellent results and 29% good results in lateral pinning case [4].
Raffi c et al. in their study found 72% excellent results and 28% good results with lateral pinning [14]. Khan obtained 88% excellent, 4% good and 4% poor results in his study [15].
In our series, the functional outcome following cross k wires was excellent in 13.33%, good in 40% of cases, fair 46.6 % and poor in 0 % and lateral pinning showed 6.6 % excellent ,46.6% good results, 40 % fair with 6.6 % poor results.
The difference in functional outcome between the two groups was not statistically significant (P=0.69). No ulnar nerve palsy occurred in our study. Skaggs et al. found no ulnar nerve palsy and no reduction was lost in 124 children managed with only lateral-entry pins [16].
Skaggs et al. noted the incidence of ulnar nerve injury as 4% in patients whom the pins were applied without hyper flexion of the elbow and as 15% in whom the medial pin was applied with the elbow hyper flexed [17]. The rate of ulnar nerve injuries varies in different studies. Lyons et al. have reported this number as 6%, Royce et al. as 3%, Agus et al. as 58% [18,19,20].
No Pin tract infection occurred in our series. In the series by Mostafavi and Sperothe incidence of pin tract infection was 5% [9]. The incidence of infection was 2% in Pirone et al. which was found more compared to our study [21].
No pin migration or significant loss of reduction was seen in our study. Gordon observed pin migration in 6% of cases and Lee noticed the loss of reduction in 7% of cases. [22,12]
Conclusion
Cross K wire or lateral K wire, both are similar in effect for the final functional outcome with no significant difference for treatment of Gartland type III supracondylar humerus fracture in pediatric age group, although taking into consideration the ulnar nerve injury, lateral k wire technique has an upper hand, but at the cost of slight loss of reduction. However, it depends upon the surgeon’s practice and preference which may negate these complications. Hence, in our study, we found lateral k wire and cross k wire equally good in terms of safety and efficacy, but stability is more in cross wires.