Introduction
Bone infarction is a term, referred for osteonecrosis of bone involving its metaphysis or diaphysis. Necrosis is an irreversible cell injury leading to death of cellular elements of bone and marrow, which can be recognized by microscopic alterations in the cytoplasm (becomes eosinophilic) as well in nucleus as, swelling, pyknosis, karyorrhexis, karyolysis. Bone infarction results from ischemia due to any cause, which can lead to destruction of bony architecture, pain and loss of function [1].
Bone infarctions may have numerous causes and have fairly distinctive imaging features on conventional radiography, CT and MRI. We have treated a case of fracture neck of femur secondary to bone infarction of left proximal femur, in a 52-year male patient, by bipolar hemiarthroplasty, with a good clinical and functional outcome. The excised head was sent for biopsy and histopathological examination.
Case Report
A 55-year-old male patient presented to us with complaints of pain in left hip since 3 and half months and inability to walk for 1 month. The pain was insidious in onset, continuous and dull-aching in nature. There was no radiculopathy, no associated fever or other constitutional symptoms. He hadn’t taken any treatment for that. After a couple of months, once while getting off from bed, he felt a jerk at left hip, following which the pain increased in severity and patients wasn’t able to stand or walk without support. The patient continued with this disability for a month, before coming to our, outpatient department.
General and systemic examinations were normal. Local examination revealed diffuse mild deep tenderness over anterior and lateral aspect of left hip with no signs of external injury. No skin changes were noted. Range of motion of the hip was terminally painful and restricted. Routine AP and lateral radiographs of hip joint and AP radiograph of pelvis with both hips (Fig 1) revealed fracture neck of femur which was subcapital type, with some subchondral sclerosis and abnormal radio-opaque lesions in the neck and inter trochanteric area.
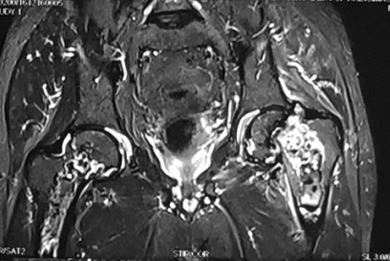
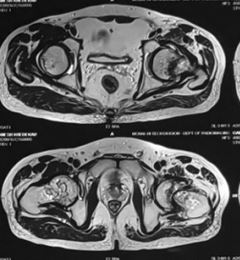
As there was no history of any high energy trauma, a pathological fracture was suspected, which needed a Magnetic resonance imaging (MRI) of both hips for further evaluation. MRI (Fig 2) showed a geographical T1 hyperintense, STIR hypointense lesions with peripheral hypointense T1 rim, in the visualized upper/mid shaft of both femurs, intramedullary in location and most likely representing bone infarcts. There was transverse pathological neck fracture of left femur without any soft tissue association. Rest of the bony skeleton, including articular margins of both hips was normal. Cemented bipolar hemi arthroplasty was planned for fracture neck femur. A standard posterior approach to hip was used, hip dislocated posteriorly and head removed using the corkscrew. Preparation of adequate calcar (approximately 1 cm above the lesser trochanter) was done using the nibbler, instead of osteotome as the bone was very brittle.
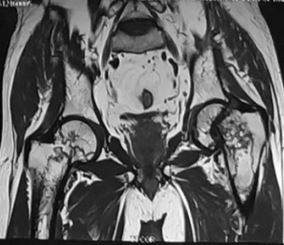
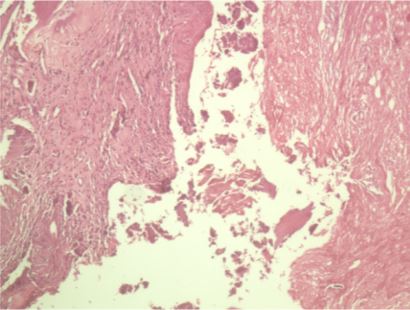
Femoral canal was prepared using canal opener and box chisel. The prepared medullary cavity was filled from bottom to top with a cement using cement gun. The prosthesis of appropriate sized head was inserted before cement got hardened, with correct rotation and valgus alignment. The hip was then reduced after the cement got set. Complete reduction, stability, and range of motion was then confirmed. The head was removed completely as a sole mass and sent for histopathological examination. Post-operative x-rays (Fig 3) confirmed proper placement of the prosthesis within the acetabular cavity. Histopathological examination (Fig 4) of femoral head showed fragments of cortical and trabecular bone. Non-viable necrosed bone with osteoid formation, fibrosis and vascular congestion with inflammatory granulation tissue was seen at places. There was no evidence of tumorous growth. The findings were consistent with a diagnosis of bone infarct in femoral head. The patient was advised abduction pillow support for post-operative period. Partial weight bearing walking with support was started after day 5. The pain was relieved, and complete range of motion of the joint was achieved within a month. There were no symptoms of sciatic neuropathy. At the last follow-up at one and half year, the patient remained free of symptoms and was satisfied with the outcome of the surgery.
Figure 1: (Radiographs)