Use of Double Bone Graft to Stabilize Prosthesis in Uncemented Partial Hip Replacement in Elderly Patients with Fracture Neck of Femur
Varma H S1, Pandey KK2*, Peepra D3, Rajpoot MS4
1 Varma H S, Department of Orthopaedics, NSCB Medical College, Jabalpur, Madhya Pradesh, India.
2* Krishna Kumar Pandey, Associate Professor, Department of Orthopaedics, NSCB Medical College, Jabalpur, Madhya Pradesh, India.
3 Peepra D, Department of Orthopaedics, NSCB Medical College, Jabalpur, Madhya Pradesh, India.
4 Manish S Rajpoot, Department of Orthopaedics, NSCB Medical College, Jabalpur, Madhya Pradesh, India.
Background: Partial hip replacement (cemented or uncemented) is the frequently done surgery in elderly patients with fracture neck of femur. Problems with cementing techniques are reported like increased infection rate and cardiac problems particularly in elderly patients with compromised cardiopulmonary reserve. Austin Moore prosthesis has its own complication like femoral loosening and frequent revision.
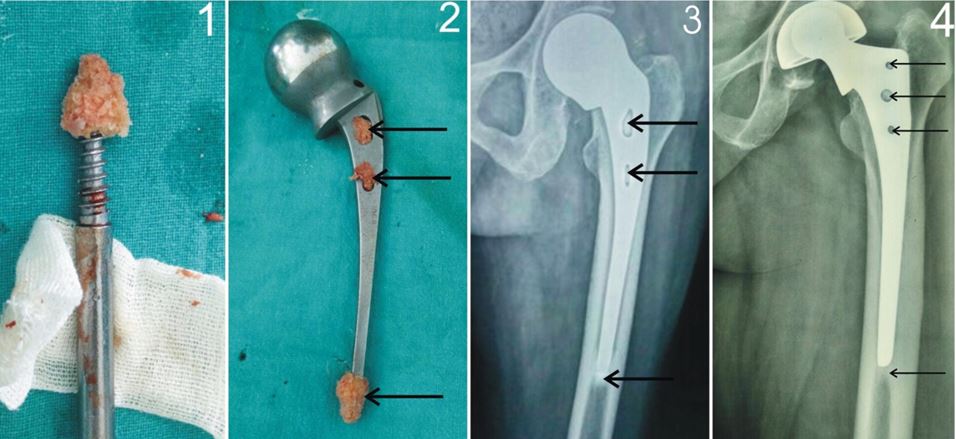
Material and Methods: We analysed results of 30 patients of fracture neck femur with Dorr type A and B proximal femoral morphology, treated by uncemented partial hip replacement (20 patients with Austin Moore prosthesis,10 patients with bipolar prosthesis) in elderly age group ( range 60 to 75 years) where double bone graft were used for additional stabilization of the stem of prosthesis in femoral canal which included transverse peg grafts in fenestrations and conical graft over the tip of the stem of prosthesis to centralise the stem.
Results: The mean follow up was 9.3 years (range from 2 to 15 years). According to Harris Hip score, final outcome was excellent in 21 hips, good in 7 hips and poor in 2 hips.Prosthesis subsidence was found in uncemented partial hip replacement with mean of 2.5 mm (range from 0 mm to 3.5 mm ) which was well tolerated due to bone plugs formed around the tip and fenestrations of prosthesis except in one patient who had complained of thigh pain which required revision with cemented modular prosthesis subsequently. Groin pain was reported in another one patient due to acetabular erosion which required cemented total hip replacement subsequently. There was no incidence of hip dislocation.
Conclusions: Our study shows that in addition to the transverse bar by fenestration grafts, bone block formed around the tip of the stem by conical graft provided strong pillar support and once it is integrated, it prevents excessive subsidence of the prosthesis with excellent result.
Keywords: Uncemented Bipolar prosthesis, uncemented Austin Moore Prosthesis, Double Bone graft
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Department of Orthopaedics, NSCB Medical College, Jabalpur, Madhya Pradesh, India. Email: |
Varma H S, Pandey KK, Peepra D, Rajpoot MS, Use of Double Bone Graft to Stabilize Prosthesis in Uncemented Partial Hip Replacement in Elderly Patients with Fracture Neck of Femur. ojmpc. 2016;22(2):37-41. Available From https://ojmpc.com/index.php/ojmpc/article/view/37 |