Introduction
Fractures of the shaft of humerus have been treated conservatively since ages. Sarmiento et al[3] since 1977 have published good results with functional cast bracing for fractures shaft humerus with residual angular deformities usually functionally and aesthetically acceptable.However conservative treatment cannot be recommended in every case.
Chapman et al [4] in their study to compare the clinical and radiographic results for locked intramedullary nail and plate reported follow-up of average thirteen months. 42 fractures (93 percent) in the Plate group were healed by 16 weeks versus 33 fractures (87 percent) in the nail group (p = 0.70). Shoulder pain and a decrement in shoulder range of motion were significant associations with nail (p = 0.007 for both variables) but not with Plate. A decrement in elbow Range of motion was significantly associated with Plate (p = 0.03), especially for fractures of the distal third of the diaphysis (p = 0.123)4.
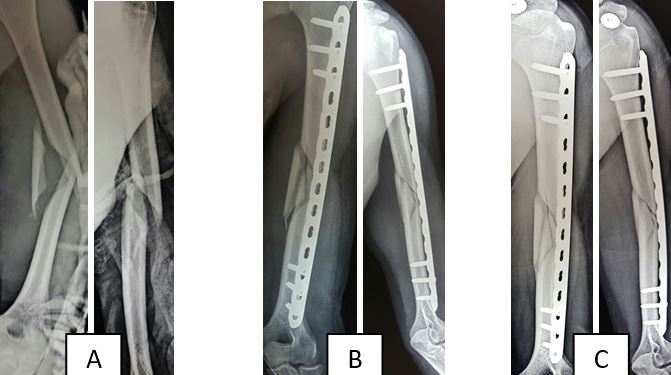
In 1996 , the concept of MIPPO was introduced by Krettek and Tscherne[5] for fractures of distal femur. Bridge plating is used to stabilize comminuteddiaphyseal fracture of long bones by an elastic construct, without an attempt to anatomically reduce the comminuted fragments,with an aim only to restore length , alignment and rotation of distal fragment in relation to proximal fragment. The elasticity of the construct allows fracture healing by callus formation,unlike rigid compression plating.A long elastic plate is able to withstand bending stresses better, as load is distributed over a longer area , so that load per unit area is less and chances of implant failure reduces considerably.
In 2005 Apivatthakakul T et al[6] explored the possibility of anterior bridge plating for shaft of humerus fractures in a cadaveric study.Since then several papers on anterior bridge plating for fractures shaft of humerus have been published in literature.
Yu, Liu et al[7] in their meta-analysis compared Bridge plating using MIPPO with conventional plate osteosynthesis, found that radial nerve injury which is as common as 6.5 % in conventional plate osteosynthesis was very rare in Bridge plating. The incidence of non-union and delayed union was also less in bridge plating.
Singisetti et al[8] compared nailing with conventional plate osteosynthesis and found no difference in outcome. There are several other studies comparing interlock nailing with conventional plate osteosynthesis but very few with Bridge plating.
KejianLian et al[9]in their study in 2013 had compared MIPPO with interlock nailing of shaft humerus fractures and found the outcome comparable in two groups. Changulani et.al [10]in their study compared the results of the humerus intramedullary nail and dynamic compression plate in 47 patients. This study proves that nail can be considered a better surgical option for the management of diaphyseal fractures of the humerus.
Early restoration of joint motion to normal physiologic function and minimal morbidity is now regarded as ideal fracture treatment. Though plate fixation has given high rates of union, it requires extensive surgery, increase chances of infection or nerve damages. Conventional nail of Kuntscher, Rush Pins, and Enders nail have been used with varied results.
These devices do not provide rotational stability; locked intramedullary nailing technically avoids these problems by transverse locking screws at each end, thus allowing early mobilization. Specially the shaft fractures with severe comminution and bone loss can be effectively treated by this method. The treatment ofcomminuted humeral shaft fractures, the choice of bridge plating or Intramedullary nailing remains controversial.
Aims and Objective
To compare and analyse outcome of treatment of comminuteddiaphyseal fracture humerus by interlocking nail with bridge plating in terms of –Early mobilization, Range of Movement, Size of incision, Hospital stay, Number of antibiotic dosage, Blood loss, Fracture healing, Complications.
Material and Methods
The study was conducted in the Department of Orthopedics, Traumatology and Reconstructive surgery Sri Aurobindo Medical College and Post Graduate Institute, Indore on total 30 patients, 15 for nail and 15 for bridge plate, from September 2012 to September 2014.
Inclusion criteria: Age: >18 yrs, Both sex, Humeral shaft fractures treated within 1week by nailing or plating, Patients with grades 1 and 2 open fractures, Polytrauma, Unstable fractures
Exclusion criteria: Epiphyseal plate open, Fracture line extending into the metaphysis, Patients with grade 3 compound fractures, Patients with pathological fractures, Patients with neglected fractures of the humerus.
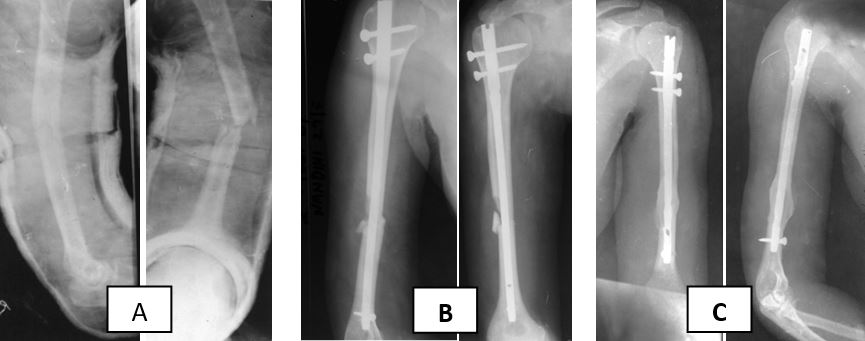
The patients presenting to the hospital with humerus diaphyseal fracture and fulfilling inclusion criteria were randomised by computer generated table and treated surgically by bridge plating or interlocking nailing. Only ante-grade nailing was done because of greater familiarity with the method among the
surgeons. From the second day, isometric exercises were carried out. For bridge plating only anterior surface of humerus was used. In all cases minimally invasive approach was used. Reduction was achieved by manual traction.
Immediate active mobilization was done in all cases. All patients were followed up in outpatient for Clinical and radiological assessment at 6weeks and at 3, 6 months. The outcomes were assessed in terms of functional outcome, ability to return to previous jobs after 6 months, union time, union rate and the incidence of complications. Functional outcome was assessed using the American Shoulder and Elbow Surgeons Score.