Demographic Characteristics of Congenital Talipes Equinovarus in Bundelkhand Area of Madhyapradesh
Choubey R1*, Kiradiya N2, Shukla J3
1* Choubey R, Department of Orthopaedics, Bundelkhand Medical College, Sagar, Madhya Pradesh, India.
2 Kiradiya N, Department of Orthopaedics, Bundelkhand Medical College, Sagar, Madhya Pradesh, India.
3 Shukla J, Department of Orthopaedics, Bundelkhand Medical College, Sagar, Madhya Pradesh, India.
Background: Most author reported the prevalence of congenital anomalies in patients with CTEV from 10 to 40%, depending on the population and method of study. The aim of our study was to determine demographic characteristic of CTEV in Bundelkhand area of Madhya pradesh. The second purpose of this study was to determine whether the Ponseti method can correct non-idiopathic CTEV with low recurrence risk, with Null hypothesis stating there was no difference between the two groups treated by Ponseti method.
Material and Methods: One hundred eight patients with one hundred and fifty-seven feet who had been treated with Ponseti’s method of casting at our institution between November 2012 to March 2016 were enrolled in this study. All the relevant data was collected that includes patient’s clinical profile including precast and post cast Pirani`s score, post treatment complications.
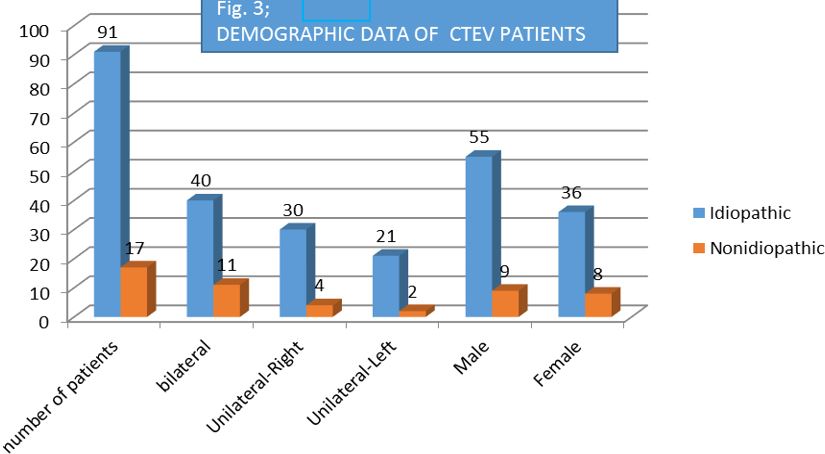
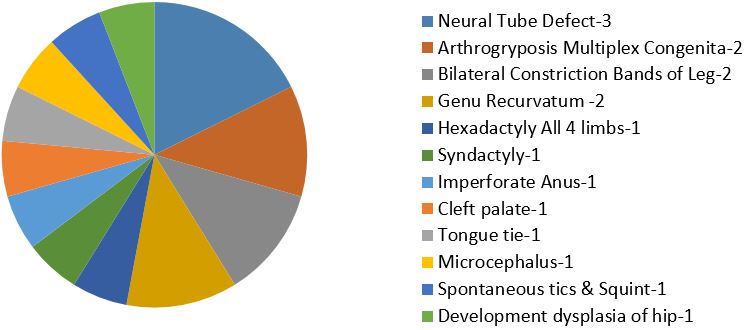
Results: Out of total of 159 feet in 108 patients (44 females, 64 males), 131 feet were idiopathic in 91 (84%) patients, whereas 28 feet were non-idiopathic in 17 (16%) patients. Idiopathic variety had 7.6% recurrence whereas non-idiopathic variety had 28.5% recurrence. On applying Chi-Square Test we concluded that null hypothesis is wrong and non-idiopathic CTEV has more recurrence rate compared to idiopathic variety.
Conclusions: In our study majority of patients with CTEV (84%) are idiopathic, 16% were non-idiopathic. We found that Ponseti method is an excellent method of correction for idiopathic clubfeet in infants. We demonstrated here that non-idiopathic CTEV can be treated with the Ponseti method with higher recurrence rates as compared to non-idiopathic variety.
Keywords: CTEV, Non idiopathic CTEV, Ponseti method of Casting
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , , Department of Orthopaedics, Bundelkhand Medical College, Sagar, Madhya Pradesh, India. Email: |
Choubey R, Kiradiya N, Shukla J, Demographic Characteristics of Congenital Talipes Equinovarus in Bundelkhand Area of Madhyapradesh. ojmpc. 2016;22(2):16-21. Available From https://ojmpc.com/index.php/ojmpc/article/view/34 |