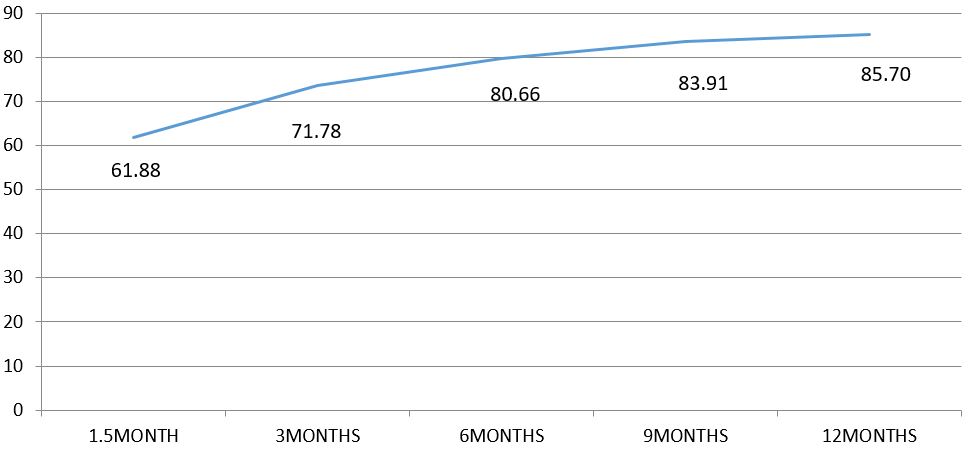
In our study, out of 44 cases which were available for final 1 year of follow up 19 patients (43.18%) achieved excellent results, 17 patients (38.63%) achieved good results, 5 patients (11.36%) achieved fair results and 3 patients (6.8%) achieved poor results. 81.81% of the patients achieved an excellent or good result.
Discussion
The aim of surgery in fracture neck femur is early return to daily activities. This is particularly applicable to the elderly age group where complications need to be prevented. The mean age of the patients in the present study was 71.6 years. Patients with hip fractures have an increased mortality rate during the first year after fracture but after one year the mortality rate is comparable to that of the general population.
The results of our study showed that age of the patient had minimal influence on the final clinical result. As in most standard studies, the present study also had a higher number of females with the left side more commonly affected than the right. Majority of our study patients (53.33%) sustained the injury due to a trivial trauma like tripping or slipping. This is a very common occurrence in elderly population where poor vision and lack of neuro-muscular coordination is a problem.
All of our study patients had a displaced fracture of the neck of femur. Majority of the patients (61.66%) had a trans-cervical fracture while 21.66% patients have sub-capital and 16.66 have basal fracture. The anatomical type of fracture and the displacement did not have any effect on the final function. Diabetes was found to be the most common co-morbidity seen in 13.33% of the study patients. All patients had Type II Diabetes and were on oral hypoglycaemic agents.
They were shifted to insulin pre-operatively and blood sugar values optimized before taking up for surgery. The other co-morbid conditions seen in the order of frequency were hypertension (31.66%), COPD (13.33%), heart disease (11.66) and ipsilateral knee osteoarthritis (10%). It was observed that the post-operative rehabilitation of patients was significantly affected by the presence of the above co-morbidities. This also had an effect on the final functional result of the procedure. Similar observations have been made by Koval et al and Bath [7,8,9].
In more than half of the cases, the blood loss was < 200ml for the whole procedure and in 23.33% of the others it was between 200-400ml. Only 13.33% of cases had a blood loss of >400 ml requiring a blood transfusion. It has been reported in literature that the average blood loss with hip hemiarthroplasty is less in the anterior approach as compared to the posterior approach.
Most of the surgeries were completed between 90-120 minutes of starting the procedure. Similar duration of the procedure has been reported by Haidukewych, et al [10] and Drinker & Murray, et al [11]. Neither the intraoperative blood loss nor the duration of the procedure had any effect on final function. Superficial infection in the form of a wound dehiscence was seen in one patient (10%) who was a diabetic.
They were managed by adequate control of the diabetic status and appropriate antibiotics based on culture-sensitivity results. The infection resolved without any sequelae and there was no late reactivation of the same. Infection rate of 3.9% after bipolar hemiarthroplasty is reported by Nottage, et al [12].
The minimum duration of hospital stay amongst the study patients was 14 days and maximum duration was 29 days with the average being 22 days. Average hospital stay of 18 days with bipolar hemiarthroplasty has been reported by Lestrange [13]. Drinker and Murray et al [11] have reported an average hospital stay of 23 days with the same procedure. There were no late postoperative complications like loosening, dislocation, erosion, secondary osteoarthritis, protrusio acetabuli or periprosthetic fracture.
We are unable to comment upon long term acetabular erosion due to relative short follow up. None of our patient reported with post-operative femoral fractures. Langslet E et al [14] reported the prevalence of post-operative femoral fractures in 0.9% with cemented hemiarthroplasty. Maricevic et al [15] reported no poor results in elderly patients with femoral neck fracture treated with bipolar hemiarthroplasty, this study has 6.8% poor results.
In a meta-analysis of 106 reports on displaced femoral neck fractures, Lu-Yao et al [9] found the incidence of reoperation within 2 years to range from 20% to 36% after internal fixation in greater than 65 years old patients. The reoperation rate after hemiarthroplasty within the same time interval was 6% to 18%. He had 33% nonunion and 16% avascular necrosis for patients treated with internal fixation. He found rate of re-operation was double when unipolar prosthesis is used.
None of our patients required revision surgery. As reported by Bhandari et al [16] in a meta-analysis of nine trials comparing arthroplasty with internal fixation in 1162 patients, found that arthroplasty significantly reduced the risk of revision surgery.
Overall, 19 patients (43.18%) had Excellent result, 17 patients (38.63%) had Good result, 5 patients (11.36%) had fair result and 3 patients (6.8%) had poor result. Overall, 81.81% of the patients had an excellent or good result. Our results are comparable with standard studies of bipolar hemiarthroplasty performed for fracture neck femur. Moshein et al [17] reported excellent results in 40% of the cases and good results in 22% of cases.
Similarly, another study by Lestrange [13] reported excellent results in 39.6% of cases and good results in 31.2% of cases. Shortcomings of this study are non-randomised, non controlled study with short follow up.
Conclusion
Cemented Bipolar hemiarthroplasty for fractures of the femoral neck in elderly gives good functional outcome as per Harris Hip Score. A randomised controlled study with long follow up can prove superiority of cemented bipolar prosthesis over other prosthesis.