Fracture Shaft Humerus: Plating OR Nailing?
Choudhari P1*, Baxi M2, Patidar S3
1* Pradeep Choudhari, Professor, Department of Orthopaedics, Sri Aurobindo Medical College and Post Graduate Institute, Indore, Madhya Pradesh, India.
2 Baxi M, Department of Orthopaedics, Sri Aurobindo Medical College and Post Graduate Institute, Indore, Madhya Pradesh, India.
3 Patidar S, Department of Orthopaedics, Sri Aurobindo Medical College and Post Graduate Institute, Indore, Madhya Pradesh, India.
Background: Conservative management of fracture shaft humerus yield in satisfactory results in most of the cases. Dilemma between dynamic compression plating and ante grade intra-medullary nailing occurs when a surgery is indicated.
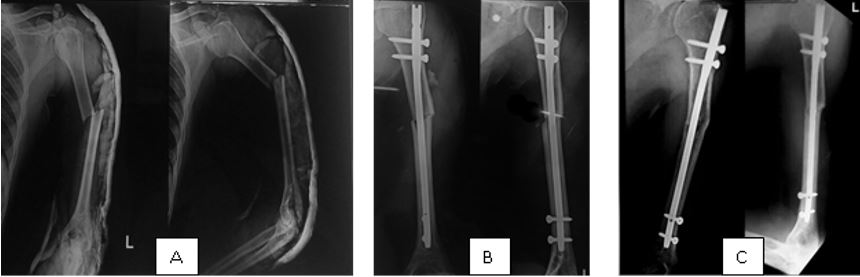
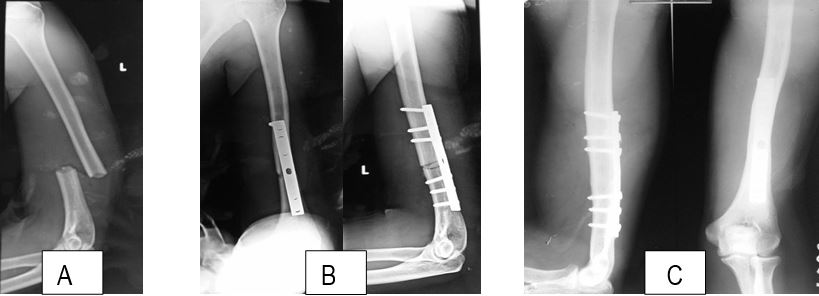
Method: A total of 42 patients with fracture shaft humerus were treated surgically. 22 were subjected to plating and 20 were subjected to intra-medullary nailing. Functional outcome of patients were recorded using Constant and Murley score along with other parameters such as duration of surgery, intra-operative blood loss, complications and union time.
Results: Mean duration of surgery in plating group was 125.13 minutes and in the nailing group was 51.95 minutes. Average amount of blood loss in plating group was 209.09 ml and in nailing group was 60.5 ml. In the plating group 17 (77.27%) patients had complication free recovery period. 2 (9.09%) patients were found to have post-operative radial nerve palsy. 3 (13.63%) patients reported with superficial surgical site infection with wound dehiscence. In the nailing group 17 (85%) patients had uneventful recovery. 2 (10%) reported pain at shoulder and 1 (5%) patient complained of decreased abduction of shoulder at 1 year follow up. As per the Constant and Murley score, in the plating group 14 (63.63%) patients yielded excellent, 4 (18.18%) good, 2 (9.09%) fair and 2 (9.09%) poor results. Whereas, in the nailing group 14 (70%) patients yielded excellent, 4 (20%) good, 1 (10%) fair and 1 (10%) poor results. Mean radiological union time in plating group was 15.63 weeks and in the nailing group was 14 weeks.
Conclusion: Both intra-medullary nailing and dynamic compression plating are excellent methods for surgical fixation of shaft humerus fractures. Both of these methods yield in comparable results in terms of functional outcomes and union rates. Intra-medullary nailing holds edge over plating in terms of lesser blood loss, lesser operative time, shorter stay in hospital and less incidence of complications such as radial nerve palsy.
Keywords: Shaft humerus, dynamic compression plate, intra-medullary interlocking nailing
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Professor, Department of Orthopaedics, Sri Aurobindo Medical College and Post Graduate Institute, Indore, Madhya Pradesh, India. Email: |
Choudhari P, Baxi M, Patidar S, Fracture Shaft Humerus: Plating OR Nailing?. ojmpc. 2016;22(1):8-14. Available From https://ojmpc.com/index.php/ojmpc/article/view/21 |