Results
In the present study, a comprehensive analysis of the available data yielded several key findings. The mean age of the cases was 38 years, with a range from 17 to 67 years. Out of the 10 cases examined, 8 were males and 2 were females. Fractures were distributed evenly between the left and right lower extremities, with 5 cases on each side. The majority of cases (60%) resulted from road traffic accidents, while 30% were attributed to falls from altitude, and 10% were caused by heavy objects.
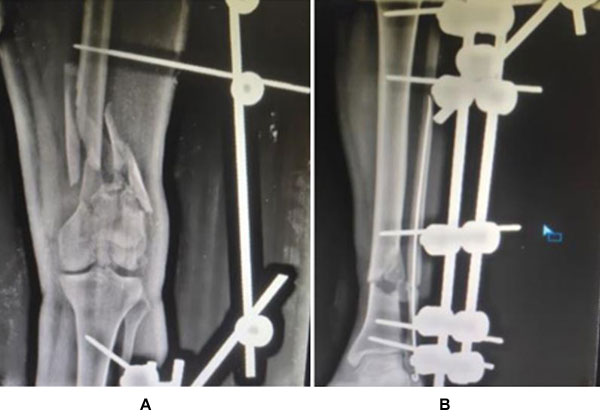
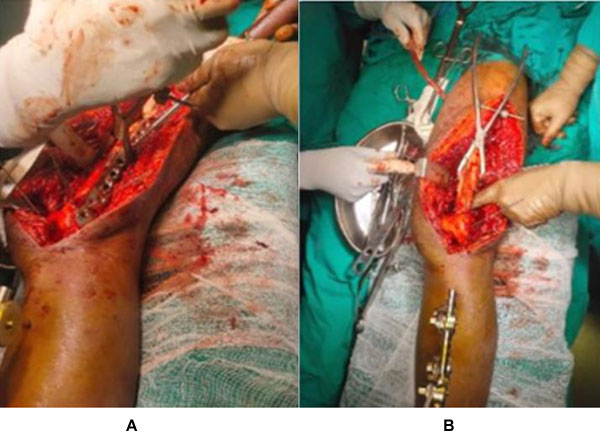
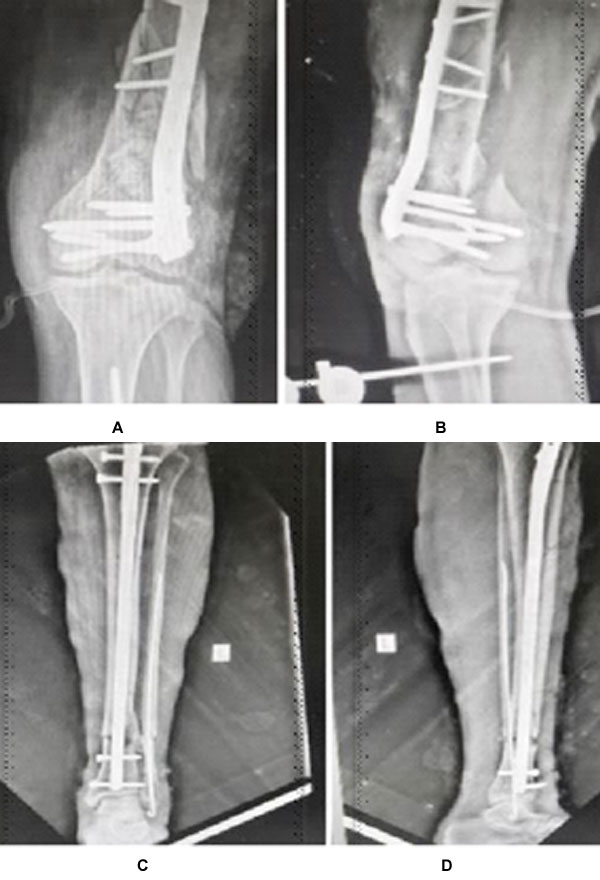
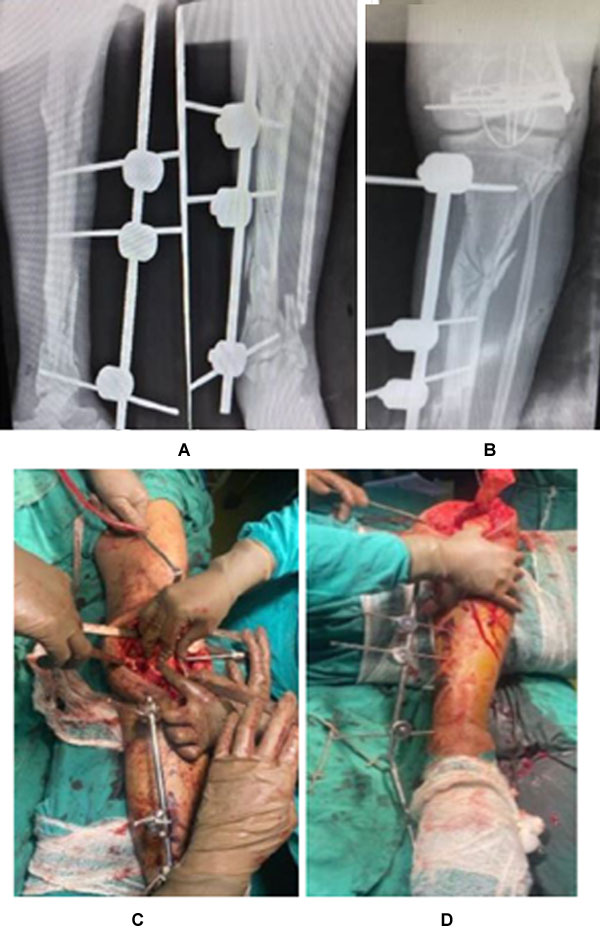
Regarding treatment, both intramedullary nails and plates were utilized for femoral and tibial fractures, with each method employed in 5 cases. Concomitant injuries were observed in 7 cases, adding complexity to the management approach. Notably, 50% of tibial fractures and 40% of femoral fractures were classified as open, with Gustilo type II being the most common subtype in both cases. Evaluation at the 6-month follow-up revealed promising outcomes, with 80% of cases achieving excellent to good results according to the Karlström–Olerud scoring system. However, 10% of cases demonstrated acceptable results, while 10% exhibited fair to poor outcomes, underscoring the challenges inherent in managing these complex injuries.
Discussion
The prognostic indicators in floating knee cases encompass associated injuries and the type of fracture, whether it's open, intra-articular, or comminuted. Achieving a favourable final outcome necessitates the proper management of associated injuries, employment of external fixation, intramedullary nailing for both fractures, plate osteosynthesis and combination of implants. Notably, optimal results were attained when both fractures underwent intramedullary nailing, facilitating an earlier return to normal activity levels compared to alternative treatment approaches. Many surgeons regard the type of fracture (open, intra-articular, comminuted) and the severity grade of soft tissue and associated injuries as crucial prognostic indicators for both initial and final outcomes in patients with floating knee injuries. These factors represent significant risks for unfavourable outcomes in such cases. Through multivariate analysis, certain studies have identified intra-articular involvement of the knee joint as a significant contributing factor affecting the final outcome of floating knee injuries. Within these variables, the Fraser type plays a pivotal role in determining the ultimate result, with knee involvement considered the most influential factor. Some studies have shown poorer outcomes when one or both fractures involve the joint compared to cases where both fractures are diaphyseal. According to the Blake and McBryde classification, type I cases tend to have better outcomes, whereas type II cases typically exhibit comparatively poorer outcomes, likely due to articular injury and knee stiffness following prolonged protection.
In a study by Rethnam et al., 29 patients with floating knee injuries were managed over a 3-year period. The mechanism of injury was RTA in 27 patients. There were 38 associated injuries.
Twenty patients had intramedullary (IM) nailing for both fractures. The complications were knee stiffness, foot drop, delayed union of tibia, and superficial infection. The mean age of the study group was 28 years (18-56). The right side was involved in 19 and left side in 10 patients. There were 20 Type 1, 3 Type 2A, and 6 Type 2B floating knee injuries according to the Fraser classification. Results of this study showed that the frequency of injured men was higher than in females and the most common cause of injury was vehicle accidents. It was also shown that almost half of the patients were in the age group of 20-29. (8)
Dwyer showed that the middle third of the shaft of both femur and tibia was most commonly (75%) involved, as in other reports. Concomitant injuries were common and were observed in 40 of the 60 patients, and delayed mobilization in all of them. A higher percentage (27%) of patients underwent amputations compared with the maximum of 25% in other studies (5). The reported incidence of open fractures is consistently high, 57% to as high as 81%. The most common pattern is an open tibial and closed femoral fracture. The obviously deformed and bruised limb is easily distracting. Associated trauma to the head, chest, abdomen, pelvis, and long bones of contralateral extremity is common. The reported rate of such injuries may be as high as 89%, highlighting violence involved. (6) In largest series reported till date by Kao et al., 110 (26%) patients had head injury, 37 (8.8%) had pelvis fracture, and 230 (55%) had contralateral serious extremity injury. Surprisingly, incidence of vascular injury is reportedly low (7). Paul et al. reported (29%) vascular injuries in their series of 21 patients (9). This high rate was, however, not shared in larger studies. Kao et al. in fact, did not comment on vascular insult in their report on 419 patients. (7) Most of injuries to head, chest, and abdomen were life threatening. Adamson et al., in their study, encountered 71% major associated injuries with 21% vascular injuries. The reported mortality rate ranged from 5% to 15%, reflecting seriousness of associated injuries. (10)
Piétu et al., in a retrospective analysis of 172 cases according to the Fraser classification, reported that 71.5% of the cases were type I and the repartition of the type II in the three subgroups was as follow: II A 8.2%, II B 11.6%, and II C 8.7%. At least one of the fractures was open in 69.2% of the patients. The average Injury Severity Score (ISS) was 19.5. The polytraumatized patients (ISS over 18) represented 37.7% of cases. The surgical procedure started within 6 first hours in 62% of injured people. The Intramedullary nailing was preferred method at femur site (73%, 126 cases), tibia Intramedullary nailing was performed in 54.4% of cases, and external fixation was used in one in every four patients. (11)
In a study by Abalo et al. on 43 patients with floating knee injuries, results showed that there were 32 males and 11 females with a mean age of 37 years. All patients had sustained their injuries in motor vehicle accidents. According to Fraser's classification, there were 21 type I, 10 type IIa, 7 type IIb, and 5 type IIc. The complications encountered were 1 case of fat embolism, 8 cases of knee stiffness, 10 cases of delayed union, 9 cases of infections, and 7 cases of nonunion. (12)