Functional and radiological outcome of locking compression plate for distal end radius fracture
Patidar A1, Jadhav A2*, Jain A3, Bhinde S4, Singh V5, Rathore S6, Sharma S7
1 A Patidar, Department of Orthopaedics, RD Gardi Medical College, Ujjain, Madhya Pradesh, India.
2* Aditya Jadhav, Senior Resident, Department of Orthopaedics, RD Gardi Medical College, Ujjain, Madhya Pradesh, India.
3 A Jain, Department of Orthopaedics, RD Gardi Medical College, Ujjain, Madhya Pradesh, India.
4 S Bhinde, Department of Orthopaedics, RD Gardi Medical College, Ujjain, Madhya Pradesh, India.
5 V Singh, Department of Orthopaedics, RD Gardi Medical College, Ujjain, Madhya Pradesh, India.
6 SS Rathore, Department of Orthopaedics, RD Gardi Medical College, Ujjain, Madhya Pradesh, India.
7 SK Sharma, Department of Orthopaedics, RD Gardi Medical College, Ujjain, Madhya Pradesh, India.
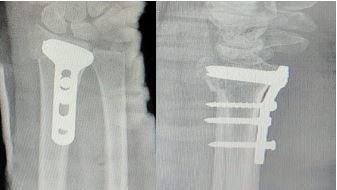
Background: Fracture distal end of radius are one of the most common skeletal injuries encountered in orthopaedic departments. Various modalities for treatment like close reduction and cast application, external fixators, ORIF with plate etc. Close reduction and cast application or K-wire fixation, external fixation is associated with immobilisation, wrist stiffness, loss of reduction postoperatively. So, we performed volar plating for distal end radius fractures and assessed the results.
Study design: Prospective case series of 48 patients who underwent volar plating for distal end radius fracture at CRGH associated with R D Gardi Medical College, Ujjain.
Methods: We performed ORIF with plating (Volar approach) in 48 patients (32 male and 16 female) of distal end radius fractures, depending on inclusion and exclusion criteria. Fractures were classified according to Frykman classification. All patients were operated under tourniquet and anaesthesia. Results were analysed using Green and o'brien scores for functional and Lidstrom classification for radiological outcome.
Results: Out of 48 patients, as per Frykman classification 1 had type III, 30 had type IV, 7 had type V,8 had type VI and 2 had type VII fractures. RTA as a (52.1%) mode of trauma was higher as compared to Fall (47.9%). Average time to clinico-radiological union was 8 weeks with the longest follow up time 6 months. Average time to wrist mobilisation was 8 days. According to Green and o'brien scores, 22 patients had excellent,20 good and 6 fair results. As per Lidstrom classification 26 patients had excellent,18 good and 4 fair results.
Conclusion: Volar plating for fracture distal end radius reduced the chances of wrist joint stiffness, loss of reduction and good results increased the patient compliance.
Keywords: distal end radius fracture, Volar plating, locking compression plate
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Senior Resident, Department of Orthopaedics, RD Gardi Medical College, Ujjain, Madhya Pradesh, India. Email: |
Patidar A, Jadhav A, Jain A, Bhinde S, Singh V, Rathore S, Sharma S, Functional and radiological outcome of locking compression plate for distal end radius fracture. ojmpc. 2022;28(2):75-82. Available From https://ojmpc.com/index.php/ojmpc/article/view/162 |