Introduction
Fracture of the proximal humerus comprise nearly 4% of all fracture and 26% of fracture of humerus (1).They are the commonest fracture in elderly population, which ranks the third and the first and second being, hip and distal radius fracture respectively. Proximal humerus involves head, greater tuberosity, lesser tuberosity and proximal one fourth of the shaft.(2) Mostly common in elderly patients due to osteoporosis and less frequently in young adults due to high energy trauma. Usually high energy trauma associated with dislocation.(3)
These types of fractures are very challenging for treatment because of its osteoporotic quality in the elderly people and the deforming forces of the muscles attached. Most of proximal humerus fracture in younger as well as in the elderly patients, are stable & slightly or non-displaced , can be treated non operatively (2).These comprise nearly 80% of proximal humerus fracture. The rest of 20% requires surgical fixation either because they needs better shoulder mobility or because their fracture is more severe.(4)
Neer's classification distinguishes between the number of displaced fragments with displacement defined as greater than 45° of angulation or > 1 cm of separation. These types of fracture require stable fixation. There are different types of fixation for proximal humerus fracture like k-wires, screw fixation, T-buttress plate, conventional plate, locking plate and prosthetic replacement. Every fixation has its own complication. The proximal humerus with poor cancellous bone quality especially in older patients, results in high risk of failure of fixation with conventional Plating system.(5)
The multiple k-wire has been introduced to reduce these complications especially in older osteoporotic individual. Even minimally displaced fracture can be treated with transcutaneus pinning to early mobilize the fracture in elderly patient, thereby to avoid shoulder stiffness. Highly communited 3 & 4 parts fracture in elderly pt can be fixed with transcutaneus pinning and thereby enhance the functional out come. This study enlightens the functional outcome & management of the fracture in elderly patient of humerus involving the proximal part, with transcutaneus pinning.
Material and methods
A prospective study was performed at Department of Orthopaedics and Trauma Centre in J. A. Group of Hospitals, Gwalior (M.P.) on all patients diagnosed with intra-articular proximal humerus fracture presenting to us from November 2018 to June 2022. Fractures were classified according to Neer’s classification for proximal humerus fractures(6). Only closed, displaced two- or three-part fractures and patients of age more than 45 years were included in the study. A written informed consent was obtained from all the patients for inclusion in the study. Patient demographics, injury mechanism was noted and clinical assessment was done. Radiographic evaluation was done with anteroposterior and axillary radiographs of shoulder.
Fractures were managed by close reduction and percutaneous pinning with K wires. Fracture pattern included for study will be fracture of proximal Humerus. Selection based on some inclusion and exclusion criteria.
Inclusion Criteria was all skeletally mature patients presenting with displaced proximal humerus fracture according to NEER two-, three- and four-part fracture in elderly patients, closed fracture of proximal humerus, Age > 45 Years, patients who have given consent to this study, patients with complete clinical records, preoperative ambulatory patient and medically unfit patients (under short Anesthesia).
Exclusion Criteria was age group (<45yr age), pathological fracture from primary or metastatic tumours, undisplaced fracture, fracture associated with neurovascular deficits, shaft humerus fracture with proximal extension, Neer’s one part fracture, refusal to consent and preexisting Shoulder pathology technique(7).
Cases were operated in routine hours and emergency as per admission and availability of Operation Theater. Most of the cases can be operated between 2nd to 10th day of admission.
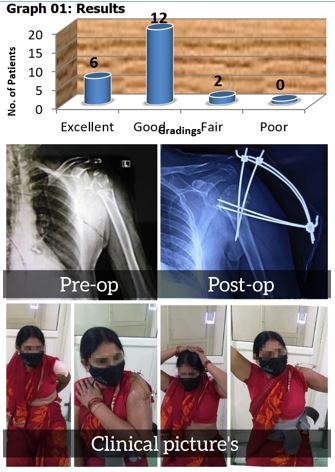
After preoperative assessment cases were posted for surgery. Under aseptic precaution and prophylactic antibiotic coverage, cases were operated with multiple k wires for proximal humerus fracture, in randomized group. Data collection procedure was included detailed study variable like preoperative and post operative clinical, radiological, surgical and functional status of involved extremity. Data collection tools had patient proforma and questioners table to show patients detail of examination, preoperative workup and surgical methods and post operative follow up. Questioners table was used for functional outcomes.
A through history was obtained including mechanism of injury and patients overall medical status, age and function and economical demands. The functional outcomes and clinical results of the patients evaluated & graded using following criteria.
In the case of a two-part surgical neck fracture, or a three-part fracture in which there is significant displacement of the shaft from under the humeral head, a trial reduction is performed to confirm the feasibility of closed reduction and percutaneous fixation. Reduction is performed by applying longitudinal traction with the arm in minimal abduction and some flexion. In case the humeral shaft is anteriorly angulated or displaced, it can be reduced by posterior pressure at fracture site lifting elbow upwards. For varus angulation a lever can be placed through a small incision into the fracture site and maneuvered to reduce it. Alternatively, two pins can be passed into head and joy sticking can be done. A 2.5-mm terminally threaded pin is held over the shoulder, and a fluoroscopic AP image is obtained. The pin is positioned over the humeral head, coming from the lateral humeral shaft into the head. A small incision is then made over the lateral arm at the level determined by the fluoroscopic image, and an artery forceps is used to spread the soft tissue down to the humeral shaft.