Functional outcome of patients of intertrochanteric femur fracture treated with trochanteric fixation nail in elderly patients
Shukla R1*, Rajput R2, Soni A3
1* Rajeev Shukla, Professor, Department of Orthopaedics, Sri Aurobindo Medical College, and PG Institute, Indore, Mp, India.
2 R Rajput, Department of Orthopaedics, Sri Aurobindo Medical College, and PG Institute, Indore, Mp, India.
3 AK Soni, Department of Orthopaedics, Sri Aurobindo Medical College, and PG Institute, Indore, Mp, India.
Background: Intertrochanteric fractures are disabling injuries in geriatric population and they are the most frequently operated fracture type which has the highest postoperative fatality rate of all surgically treated fractures. The objective of the study was to evaluate the functional outcomes of intertrochanteric fractures treated with trochanteric fixation nail (TFN) in elderly patients.
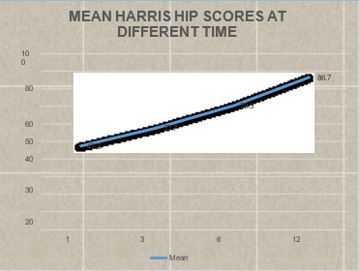
Method: This is a prospective and retrospective study with 30 patients of Intertrochanteric femur fractures carried out in the Department of Orthopaedics, Sri Aurobindo Medical College, and P.G. Institute, Indore from Jan 2015 to Aug 2020. Data collected according to Evan’s classification. Patients were followed up at intervals of 6 weeks,12 weeks,6 months and 12 months and final results were evaluated using Harris hip score at the end of 1 year.
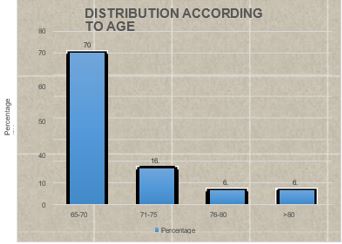
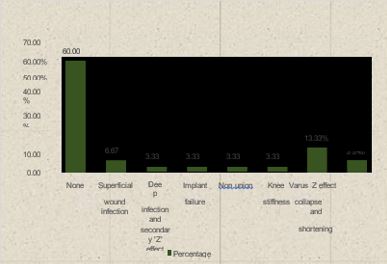
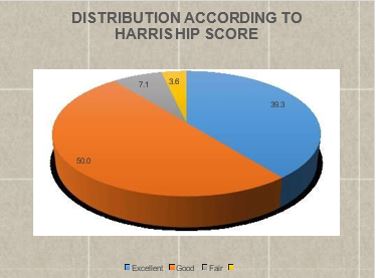
Results: The study included 30 patients, 18 males, 12 females with mean age of 70.27 years (range: 65-85 years). The fracture union rate was 96% and average union time was 12.9 weeks. Our results were excellent (39.3), good (50%), fair (7.1%) and poor (3.6%). The most common complication encountered was Varus collapse and shortening seen in 4 (13.33%) patients, superficial wound infection in 2 patients (6.67%); Varus collapse and shortening and Z effect and screw revision was seen in 2 (6.67%) while Deep infection and secondary ‗Z‘ effect, Implant failure, Non-union, Knee stiffness in 1 patient each.
Conclusion: The treatment of intertrochanteric fractures with TFN had a more favourable outcome and it is the ideal implant of choice for intertrochanteric fractures at present.
Keywords: intertrochanteric fracture, trochanteric fixation nail (TFN), Z effect
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Professor, Department of Orthopaedics, Sri Aurobindo Medical College, and PG Institute, Indore, Mp, India. Email: |
Shukla R, Rajput R, Soni A, Functional outcome of patients of intertrochanteric femur fracture treated with trochanteric fixation nail in elderly patients. ojmpc. 2022;28(2):70-74. Available From https://ojmpc.com/index.php/ojmpc/article/view/158 |