Graft Options for Anterior Cruciate Ligament Reconstruction-choose wisely
Vijayan S1, Hegde N2, Kulkarni MS3*, Aroor M4, Bhat V5, Rao S6
1 S Vijayan, Department of Orthopaedics, Kasturba Medical College Manipal Academy of Higher Education, Manipal, Karnataka, India.
2 N Hegde, Department of Orthopaedics, Kasturba Medical College Manipal Academy of Higher Education, Manipal, Karnataka, India.
3* Mahesh Suresh Kulkarni, Ms Ortho Assistant Professor, Department of Orthopaedics, Kasturba Medical College Manipal Academy of Higher Education, Manipal, Karnataka, India.
4 MN Aroor, Department of Orthopaedics, Kasturba Medical College Manipal Academy of Higher Education, Manipal, Karnataka, India.
5 V Bhat, Department of Orthopaedics, Kasturba Medical College Manipal Academy of Higher Education, Manipal, Karnataka, India.
6 SK Rao, Department of Orthopaedics, Kasturba Medical College Manipal Academy of Higher Education, Manipal, Karnataka, India.
Background: Anterior cruciate ligament (ACL) tear constitutes a major chunk of post-traumatic knee injury leading to long term functional knee impairment and reduced quality of life. Globally, an increase in the incidence of reconstructive procedures for the torn ACL have been reported with varying outcome. This has revolutionized the techniques primarily aimed at achieving a functionally stable knee joint and early return to their pre-injury level of activities.
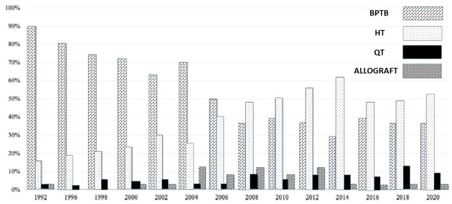
Discussion: Among the various factors which have influenced the outcome of the ACL reconstruction (ACLR), the choice of graft is a highly studied and yet still exceedingly debated topic. A large number of studies comparing the various graft options in ACLR has been published throughout the years. The purpose of this comprehensive review is to summarize the most recent relevant literatures on ACL graft options, on-going research and to discuss whether one graft type demonstrates clinical superiority over the other.
Conclusion: Understanding the biomechanical characteristics of various grafts available for anterior cruciate ligament reconstruction would help the surgeons in thoughtful selection of the graft for each patient on an individual basis and facilitate a thorough discussion between the surgeon and the patient which is vital in decision making.
Keywords: Anterior cruciate ligament; Graft; Reconstruction; Bone-patella; Hamstring; Peroneus; Quadriceps
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Ms Ortho Assistant Professor, Department of Orthopaedics, Kasturba Medical College Manipal Academy of Higher Education, Manipal, Karnataka, India. Email: |
Vijayan S, Hegde N, Kulkarni MS, Aroor M, Bhat V, Rao S, Graft Options for Anterior Cruciate Ligament Reconstruction-choose wisely. ojmpc. 2022;28(1):18-26. Available From https://ojmpc.com/index.php/ojmpc/article/view/149 |