Introduction
Congenital pseudoarthrosis of tibia (CPT) is a very rare condition, with incidence of about 1 in 25000 live birth [1]. It is most commonly associated with neurofibromatosis type 1 in more than 50 % of the cases [1]. It has also been associated to fibrous dysplasia or Campanacci’s osteofibrous dysplasia [2].
Loss of neurofibromin protein and presence of hamartomas are the primary pathologies in neurofibromatosis that prevents osteoblastic differentiation, bone remodeling or fracture healing. The soft tissue at the pseudarthrotic site is composed of variable admixture of fibrous tissue, fibrocartilage, and hyaline cartilage with evidence of enchondral ossification [3].
Standard methods of treatment for CPT including internal fixation with intramedullary rodding, external fixation or ilizarov fixation, vascularized fibula transfer or combinations have varied results with high rate of recurrence [4-9].
4 in 1 osteosynthesis used to treat CPT, involves creating a synostosis between proximal and distal ends of both tibia and fibula [10, 11].
We report such a rare case of congenital pseudoarthrosis tibia which failed to unite with primary surgery of ilizarov and then was successfully treated and united with four in one procedure and also reviewed the literature on the topic.
Case report
A 5-year-old female child, presented in our outpatient department, with chief complain of deformity, shortening of right leg and inability to bear weight on affected right leg since birth. The child was delivered at full term with normal vaginal delivery. She had history of full immunization as per the national immunization schedule.
Parents and child denied any other significant past medical history. Familial history was unremarkable for any other congenital disorder. As per the parents, some deformity of right leg was noticed during the neonatal period but no treatment was taken. Child achieved all milestones at appropriate age except for ambulation, which was delayed. Child had a history of trivial trauma due to fall while playing 2 months back and had been non ambulatory since then.
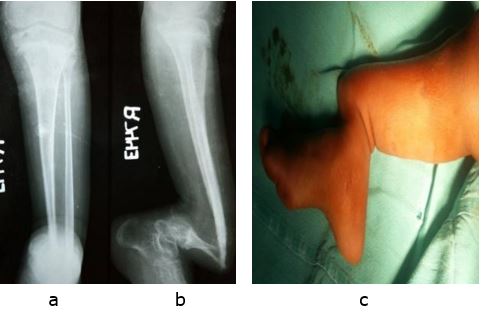
On clinical examination, distal fourth right leg was deformed with severe bowing and procurvatum deformity of about 900 (fig 1). There were clear signs of non-union of fracture of tibia and fibula with frank painless abnormal mobility present in all the planes at lower third leg. The leg musculature was severely hypotrophied. Proximal end of bone was dimpling the skin which appeared smooth and shiny.
On palpation local temperature was comparable on both sides. Distal pulsations of dorsalis pedis artery and posterior tibial arteries were palpable. Ipsilateral hip and knee examination were unremarkable but active movements of ipsilateral ankle were restricted.
Shortening of about 5 cm was present on the right side. No other deformities were seen anywhere else in the body. Routine radiographs of the limb including AP and lateral views were done which showed pencil thin severely hypotrophied tibia fibula with clear fracture at level of lower third leg.
The bone ends were atrophic and thinned out. Severe angular deformity was present at the fracture site and ankle seen in severe calcaneus position. The knee joint appeared normal.
After routine hematological work up and pre anesthetic check-up patient was primarily treated by excision of hamartomatous tissue along with ilizarov application, corticotomy and intramedullary rod fixation to achieve union and prevent refracture (Figure 2).
After 4 months of bone transport and compression at fracture site, the pseudoarthrosis failed to show signs of union, although good regenerate bone was formed at corticotomy site. Illizarov was removed and patient was planned for re-surgery with four in one osteosynthesis technique to achieve a tibio fibular synostosis (Figure 3).
Copious amount of cortico-cancellous bone graft was obtained from the ipsilateral iliac crest. Utilizing the previous incision, the pseudoarthrosis site was exposed and remnants of fibrous periosteal and hamartomatous tissue were removed (Figure 4).
Both ends i.e. proximal and distal ends of the both the bones tibia and fibula were freshened and the copious amount of cortico-cancellous auto-graft was placed between the tibia fibula to achieve a synostosis between tibia and fibula both proximally and distally. An external fixator was applied and trans-calcaneal intramedullary rush nail was also fixed to protect the union. Postoperatively, regular pin tract dressings were done.
Patient was followed regularly to confirm an uneventful postoperative period. External fixator was removed after 6 months’ post operatively. The Child achieved union at pseudoarthrosis site at 9 months, but had limb length discrepancy and is explained and planned for limb lengthening once she attains maturity (fig 5).
Figure 1:Antero-posterior (a) and lateral (b) X rays and pre-operative clinical photograph (c) of the patient showing typical features of congenital pseudoarthrosis tibia.