Efficacy of Microscopic Posterior Cervical Laminectomy for Multilevel Compressive Cervical Myelopathy: A Long Term Analysis
Asati S1, Raut S2, Ruparel S3, Patel A4, Chaddha R5, Kundnani V6*
1 S Asati, Center of Excellence in Spine Surgery, Mumbai Institute of Spine Surgery and Bombay Hospital and Medical Research Centre and Mumbai and Lilavati Hospital and Medical research Centre, Mumbai, Maharashtra, India.
2 S Raut, Center of Excellence in Spine Surgery, Mumbai Institute of Spine Surgery and Bombay Hospital and Medical Research Centre and Mumbai and Lilavati Hospital and Medical research Centre, Mumbai, Maharashtra, India.
3 S Ruparel, Center of Excellence in Spine Surgery, Mumbai Institute of Spine Surgery and Bombay Hospital and Medical Research Centre and Mumbai and Lilavati Hospital and Medical research Centre, Mumbai, Maharashtra, India.
4 A Patel, Center of Excellence in Spine Surgery, Mumbai Institute of Spine Surgery and Bombay Hospital and Medical Research Centre and Mumbai and Lilavati Hospital and Medical research Centre, Mumbai, Maharashtra, India.
5 R Chaddha, Center of Excellence in Spine Surgery, Mumbai Institute of Spine Surgery and Bombay Hospital and Medical Research Centre and Mumbai and Lilavati Hospital and Medical research Centre, Mumbai, Maharashtra, India.
6* Vishal Kundnani, Center of Excellence in Spine Surgery, Mumbai Institute of Spine Surgery and Bombay Hospital and Medical Research Centre and Mumbai and Lilavati Hospital and Medical research Centre, Mumbai, Maharashtra, India.
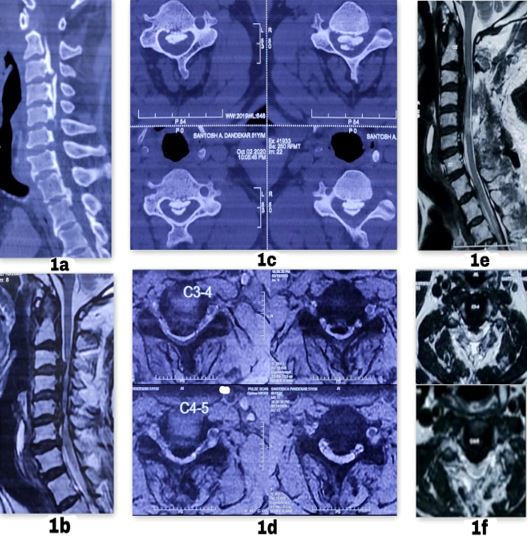
Background: Cervical spondylotic myelopathy and ossified posterior longitudinal ligament (OPLL) are the two most common causes of compressive multilevel cervical myelopathy. These may cause progressive neurological deterioration and require surgical treatment. There is no gold standard treatment available. Anterior surgery is associated with morbidity and complications in multilevel cases because of which posterior surgeries are preferred, which have shown good clinical outcomes. We determined the long-term efficacy of microscopic posterior cervical laminectomy for multilevel compressive cervical myelopathy.
Material and Methods: We reviewed 110 patients with multilevel compressive cervical myelopathy who underwent posterior cervical laminectomy from January 2007 to December 2014. Patients with age ≥45 years, C2-C7 cobb’s angle ≥ 10º, compression at ≥3 levels and a minimum of 5 years follow-up were included in the study. Demographic data, pre and post-operative clinical parameters (visual analog scale [VAS], Nurick’s grading and modified Japanese orthopaedic association [mJOA] score), radiological parameters (C2-C7 Cobb’s Angle), peri-operative parameters, complications and recovery rate were evaluated.
Results: The mean age of the patients was 55.6 years (44-74) with M: F 68:42. The mean blood loss and mean operative time was 93.9 ml and 96.6 minutes. There was significant improvement (p<0.05) in VAS (3.7±1.5 to 1.9±0.8), Nurick’s grading (3.3±0.9 to 1.8±0.6) and mJOA score (8.3±1.4 to 13.9±1.8). At final follow-up 61.8% patients’ maintained cervical lordosis, 21.8% changes to a straight spine and 16.3% became kyphotic. Intraoperatively 7 patients had a dural tear. 3 patients showed neurological deterioration postoperatively and 3 had unilateral C5 palsy which improved within 6 months period. 19% had an excellent outcome, 39% had good, 33.6% had fair and 8.1% patients had a poor outcome.
Conclusion: Microscopic posterior cervical laminectomy is the gold standard surgical procedure in patients with multilevel compressive cervical myelopathy with good recovery and clinical outcomes in properly selected patients. In long term it may causes progression of kyphosis, without any significant clinical affection.
Keywords: Cervical spondylotic myelopathy, OPLL, Cervical laminectomy, CSF leak, C5 palsy, Neurological deterioration
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , , Center of Excellence in Spine Surgery, Mumbai Institute of Spine Surgery and Bombay Hospital and Medical Research Centre and Mumbai and Lilavati Hospital and Medical research Centre, Mumbai, Maharashtra, India. Email: |
Asati S, Raut S, Ruparel S, Patel A, Chaddha R, Kundnani V, Efficacy of Microscopic Posterior Cervical Laminectomy for Multilevel Compressive Cervical Myelopathy: A Long Term Analysis. ojmpc. 2021;27(1):15-21. Available From https://ojmpc.com/index.php/ojmpc/article/view/130 |