Micro-Endoscopic Tubular Minimal Invasive Spine Surgery - Overview
Raut S1, Asati S2, Patel A3, Ruparel S4, Chaddha R5, Kundnani V6*
1 S Raut, Center of Excellence in Spine Surgery, Bombay Hospital and Medical Research Centre and Mumbai Lilavati Hospital and Medical Research Center Mumbai, Mumbai, Maharashtra.
2 S Asati, Center of Excellence in Spine Surgery, Bombay Hospital and Medical Research Centre and Mumbai Lilavati Hospital and Medical Research Center Mumbai, Mumbai, Maharashtra.
3 A Patel, Center of Excellence in Spine Surgery, Bombay Hospital and Medical Research Centre and Mumbai Lilavati Hospital and Medical Research Center Mumbai, Mumbai, Maharashtra.
4 S Ruparel, Center of Excellence in Spine Surgery, Bombay Hospital and Medical Research Centre and Mumbai Lilavati Hospital and Medical Research Center Mumbai, Mumbai, Maharashtra.
5 R Chaddha, Center of Excellence in Spine Surgery, Bombay Hospital and Medical Research Centre and Mumbai Lilavati Hospital and Medical Research Center Mumbai, Mumbai, Maharashtra.
6* Vishal Kundnani, Center of Excellence in Spine Surgery, Bombay Hospital and Medical Research Centre and Mumbai Lilavati Hospital and Medical Research Center Mumbai, Mumbai, Maharashtra, India.
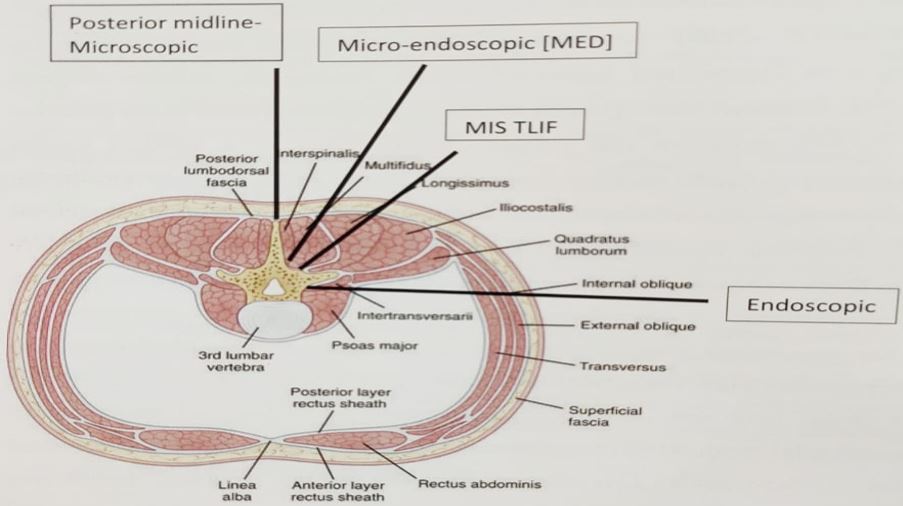
Damage to paraspinal muscles as by caused by conventional open posterior lumbar spinal surgery can lead to inferior clinical and functional results. Minimally invasive approach to lumbar spine by microscopic, endoscopic or micro-endoscopic techniques using specialised instruments via neuro-vascular planes using muscle splitting approach to accesses the pathological site can reduce or minimise these complications. MIS techniques have demonstrated less blood loss, less postoperative pain, decreased need of analgesics post operatively, faster rehabilitation, shorter hospital stays and lower infection rates as compared to open techniques. while achieving equally efficacious results.
A thorough knowledge of anatomy of posterior spinal structures and understanding of the instruments used in minimal invasive spine surgery is of paramount importance. This article focuses on the anatomy, history, basics, instrumentation and indications used in minimally invasive lumbar spine surgeries.
Keywords: Spine, Micro-Endoscopic, Minimal Invasive
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , , Center of Excellence in Spine Surgery, Bombay Hospital and Medical Research Centre and Mumbai Lilavati Hospital and Medical Research Center Mumbai, Mumbai, Maharashtra, India. Email: |
Raut S, Asati S, Patel A, Ruparel S, Chaddha R, Kundnani V, Micro-Endoscopic Tubular Minimal Invasive Spine Surgery - Overview. ojmpc. 2021;27(1):4-9. Available From https://ojmpc.com/index.php/ojmpc/article/view/129 |