Philos Plate For Fixation Of Supracondylar Dome Osteotomy
Mohindra M1, Gautam V2, Meena A3*, Gupta N4, Desai J5, Saikia S6
1 M Mohindra, Central Institute of Orthopaedics Vmmc and Safdarjung Hospital, New Delhi, India.
2 VK Gautam, Central Institute of Orthopaedics Vmmc and Safdarjung Hospital, New Delhi, India.
3* Amit Meena, Senior Resident, Central Institute of Orthopaedics Vmmc and Safdarjung Hospital, New Delhi, India.
4 N Gupta, Central Institute of Orthopaedics Vmmc and Safdarjung Hospital, New Delhi, India.
5 J Desai, Central Institute of Orthopaedics Vmmc and Safdarjung Hospital, New Delhi, India.
6 S Saikia, Central Institute of Orthopaedics Vmmc and Safdarjung Hospital, New Delhi, India.
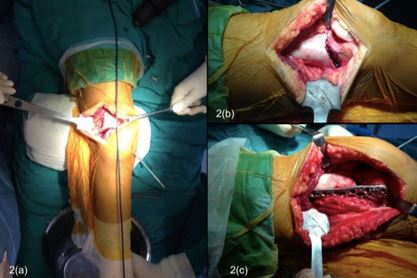
Background: Various corrective osteotomies and different modes of fixation have been described to correct genu valgum deformity. We evaluated the results of dome osteotomy for genu valgum which was stabilized with proximal humerus internal locking system (PHILOS) plate.
Material and Methods: 39 cases of Genu Valgum deformity in 24 patients treated by dome osteotomy and fixed with PHILOS plate (15 patients had bilateral deformities and 9 patients had unilateral deformity) were evaluated clinically (intermalleolar distance and tibio-femoral angle) and radiologically (tibio-femoral angle).
Results: Pre-operative mean intermalleolar distance, clinical tibio-femoral angle and radiological tibio-femoral angle pre-operatively improved from 17.5 cm (range 11 to 24), 19.250 (range 140 to 240) and 20.90 (range 150 to 260) to postoperative 2.25 cm (range 0 to 4 cm), 7.750 (range 40 to 100) and 8.950 (range 50 to 110) respectively. The mean pre-operative LDFA was 74.850 (range 670 to 830) whereas post-operative mean value was 86.90 (range 830 to 900). The mean Bostman knee score improved significantly from 20.8 (range 18 to 22) to 29.1 (range 27 to 30). 2 patients (2 limbs) had good score i.e. between 20 to 27, while rest all the patients had excellent score between 28 to 30. Improvement in intermalleolar distance, tibio-femoral angle and LDFA was statistically significant (P< 0.001)
Conclusion: Dome osteotomy with PHILOS plate fixation is reasonable cost effective, easy, available and viable option for treatment of genu valgum with excellent short to midterm results and without complication as seen by wedge osteotomy.
Keywords: Genu Valgum, Dome Osteotomy, PHILOS plate
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Senior Resident, , Central Institute of Orthopaedics Vmmc and Safdarjung Hospital, New Delhi, , India. Email: |
Mohindra M, Gautam V, Meena A, Gupta N, Desai J, Saikia S, Philos Plate For Fixation Of Supracondylar Dome Osteotomy. ojmpc. 2020;26(2):75-80. Available From https://ojmpc.com/index.php/ojmpc/article/view/122 |