Discussion
Open tibial fractures are among most common fractures in young adults encountered at various trauma centre [9-11]. As most of these patients are young adults who sustained these fractures belong to physically highly active and productive age group, they need optimal treatment to get back to their previous work capacity as early as possible and avoid long term complications.
Open tibial fractures with inherent less soft tissue coverage and added soft tissue trauma by injury poses higher risk of postoperative complications like wound dehiscence and infection [4-6]. Hence treatment of open tibial fractures demands tissue friendly surgical procedures as well as adequate fracture fixation.
External Fixator application is a commonly used technique for compound tibia fractures, its main benefit being its less invasive nature. Disadvantage of external fixator is lower stability as compared to other methods of fixation. Other limitations of the external fixator are pin tract infections, pin loosening, re-displacement, less useful in osteoporotic fracture, delayed union, non-union and malunion.
In developing country like ours, where patient load is very high and resources are limited, it is difficult getting patient into operation theatre twice especially when it is not an emergency. Irregular follow-ups, low socioeconomic group, high cost of reoperation, poor hygiene and associated pin tract infection makes conversion of temporary external fixation to definitive internal fixation, difficult [12].
Giannoudis in 96 open tibial fractures showed over 17% infection rate after conversion of external fixation to IM nailing [13]. Hence, external fixator itself is preferred as definitive treatment modality of treatment because it eliminates the second surgery, indirectly reduces the patient loads waiting for surgery and avoids the risk associated with second surgery and anaesthesia [12].
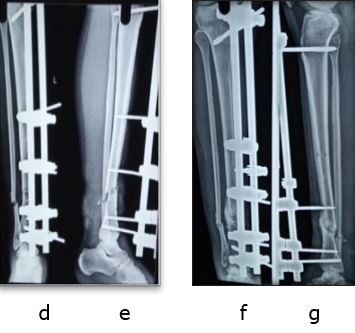
We conducted this study to confirm the role of external fixator as definitive fixation method of treatment for open tibial fractures in 57 patients with mean age 34 years and found it to be very effective with rapid healing, and few complications.
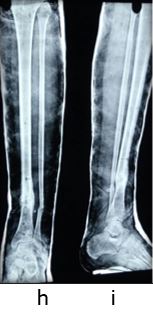
In our series, 50 (87.7%) had union, in mean time of 22.4 weeks (range 15 to 29 weeks). Similar union rate was seen by studies of Kumar (97% in 37 patients), Beltsios (91 % in 241 patients) and of Emani (95% in 62 patients) [14-16].
The mean time to union by Beltsios was 25 weeks in open fractures whereas in Emami series union time was 22 week, but 22% had delayed union [15,16].
In metaanalysis done by Bhandari et al directly comparing external fixators and unreamed IM nails, it is shown that there is no statistically significant difference between the two with respect to union, delayed union, deep infection and chronic osteomyelitis,
but external fixation was associated with statistically significant increased rate of malunion and reoperations, whereas unreamed nailing showed a statistically significant increase in the rate of failure of the implant [17].
In our study, there were 15 (18.99%) delayed union and 7 (10.94%) nonunions compared to 8 to 15% non-union and 9 to 39% delayed union in reported series by Giannoudis et al, Beltsios et al, Emani et al, Kimmel et al and Velazco A [13,15-19].
The reported incidence of malunion in Beltsios series was 1.8%, Kimmel series of 26% and Giannoudis series was 20%, but in our series only one patient (1.7%) had malunion [13,15,18].
The probable reason for this is because we tried to achieve anatomic reduction before applying the external fixator, which could have led the fracture to unite without malunion. Further, the reported incidence of pin tract infection is 32 to 80% while the incidence of deep infection is 16.2%, with average 4% developing chronic osteomyelitis [3,18,19],
but in our series we encounter 13 (22.8%) patients of pin tract infection, out of which 7 infection healed by oral antibiotics and only 6 (10.52%) requiring pin revision due to loosening. Low incidence of pin tract infection in our series is attributed to proper technique of pin insertion, preloading and adequate pin site dressing and care [20].
Thus external fixator, as a definitive treatment modality to achieve union in patients of open tibial fractures provides early and strong bone union due to inherent benefits of less tissue damage and minimal disturbance of fracture site biology.
But care must be taken to achieve proper reduction and to avoid pin related associated complications of infection / loosening by following proper pin insertion technique, pre-tensioning the pins and doing regular pin site care. For better functional outcomes range of motion, dynamization and weight bearing should be started early to promote healing by converting fixator frame to less rigid allowing axial micromovements at fracture site.
Conclusion
External fixator for compound tibial diaphyseal fractures is a very useful modality of treatment which eliminates the need of re-operation and allows bone and soft tissue healing without increasing morbidity when applied properly. Pin tract infection and loosening are common complications, but it can be reduced by proper technique.
References
1. Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24(8):742–6. [Crossref][PubMed][Google Scholar]